Article Contents ::
Diabetes insipidus (DI) Disorders of Neurohypophysis
The neurohypophysis or posterior pituitary gland is made up of nerve tissues originating in supraoptic and paraventricular nuclei of hypothalamus.
- It produces 2 hormones:
- 1. AVP or arginine vasopressin, also known as antidiuretic hormone (ADH).
- 2. Oxytocin
- AVP acts on renal tubules to absorb the water back into the circulation helping to reduce the water loss and concentrating the urine.
- AVP deficiency causes diabetes insipidus.
Diabetes insipidus (DI) —
- It is a disease of ‘Posterior pituitary insufficiency or AVP deficiency in which large amounts of dilute urine are passed.
- inadequate secretion of or insensitivity to vasopressin (ADH) leading to hypotonic polyuria.
- In excessive AVP secretion, there is decreased urine output and hyponatraemia, especially if water intake is not reduced. This is called inappropriate ADH syndrome or inappropriate AVP production.
- In DI there is urine output more than 50 mljkg in 24 hours and osmolarity is <300 mosmol / L.
- There is polyuria, urinary frequency, nocturia, fatigue, .somnolence (sleepiness), thirst, polydipsia.
Diabetes Insipidus Risk Factors
- Diabetes insipidus may be part of the paraneoplastic syndrome associated with small cell bronchocarcinoma.
- Intracranial neoplasm
- Patients using lithium
- Following surgery
- Head trauma
Causes of Diabetes insipidus (DI) are:
- · Head trauma
- · Chronic meningitis
- · SLE (Systemic lupus erythematosus)
- · Snake venom
- · Craniopharyngioma
- · Pituitary adenoma
- · Metastatic tumors
- · Pregnancy
- · Sheehan’s syndrome (post partum pituitary apoplexy)
- · Drugs like lithium, amphotericin B, aminoglycosides, rifampin
- Psychogenic Tubercular meningitis Multiple sclerosis
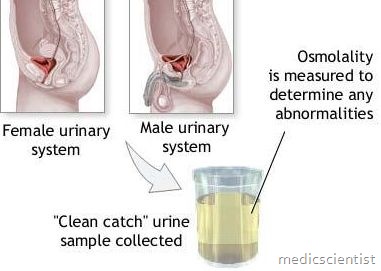
Diabetes insipidus (DI) Diagnosis —
-
Initial Lab Tests
- Plasma vasopressin or urinary vasopressin following osmotic stimulus, such as fluid restriction or administration of hypertonic saline
- Urinary glucose: Rule out diabetes mellitus.
- Normal:
- Diabetes insipidus:
- Lack of ADH activity means that urine is unable to be concentrated by the collecting ducts (urine osmolality <400 mosmol/kg).
-
Blood test :
Treatment of Diabetes insipidus (DI)
- Treatment is DDAVP – a synthetic analog of AVP.
- It increases the urine concentration, and decreases t~e urine flow.
- Other drugs are chlorpropamide (antidiabetic drug).
- Patient counselling helps in psychogenic polydipsia.
- Therapy depends on type of DI.
- ›Orally available as 0.1- to 0.2-mg tablets
- ›Intranasally 0.2–0.6 mg at bedtime
- ›Desmopressin (DDAVP) a derivative of vasopressin, available PO, nasal spray, and parenterally
- Central DI:
- ›Correct water deficits.
- ›Reduce excessive urinary water loss.
- Symptomatic nephrogenic DI:
- Amiloride can be added to HCTZ for the added effect.
- Hydrochlorothiazide 25 mg once or twice a day
- Thiazide diuretic with amiloride
- Contraindications Diabetes insipidus (DI):
- Use desmopressin with caution in the immediate postop period for intracranial lesions because of possible cerebral edema.
- Precautions Diabetes insipidus (DI):
- An overdose of desmopressin may produce water intoxication and hyponatremia in patients with excessive water intake.