Article Contents ::
- 1 Pneumonia Signs and Symptoms Pathophysiology Types of Pneumonia
- 2 Pneumonia means infection of the alveoli, distal airways, and interstitium of the lung.
- 3 Risk Factorsfor Pneumonia
- 4 History Pneumonia
- 5 Symptoms of pneumonia
- 6 Signs of pneumonia
- 7 Pneumonia Physical Exam
- 8 Chest X-ray of pneumonia
- 9 Routes of Infection for pneumonia
- 10 Pathophysiology of pneumonia
- 11 Lobar pneumonia:
- 12 Miliary pneumonia:
- 13 First stage:
- 14 Second stage :
- 15 Third stage:
- 16 Fourth stage or Final stage:
- 17 Bronchopneumonia
- 18 Interstitial pneumonia
- 19 Miliary pneumonia
- 20 COMPLICATIONS OF PNEUMONIA
Pneumonia Signs and Symptoms Pathophysiology Types of Pneumonia
clinical presentation of childhood pneumonia often is dictated by the responsible pathogen, the particular host, and the severity of the pneumonia. Inflammation of the lungs, usually due to infection with bacteria, viruses, or other pathogenic organisms. Clinically, the term “pneumonia” is used to indicate an infectious disease Bacterial infection of lung parenchyma: Community-acquired pneumonia: Acute infection of the pulmonary parenchyma in a patient who has acquired the infection in the community
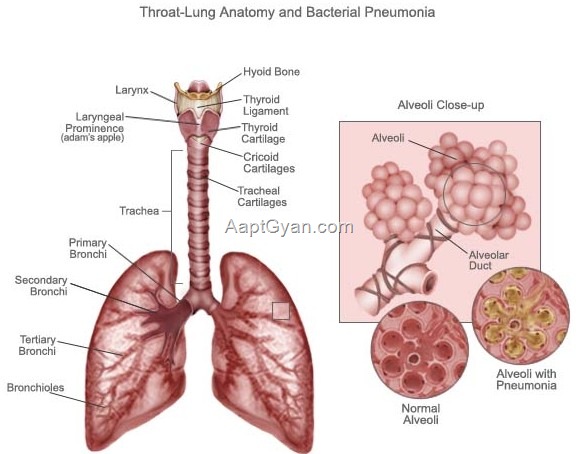
Pneumonia means infection of the alveoli, distal airways, and interstitium of the lung.
- As a result of infection there is :
- Increase in bulk of lungs
- Decreased sponginess of lungs
- Consolidation of lungs
- Air in alveoli replaced by WBC, RBC, Fibrin.
Risk Factorsfor Pneumonia
- CAP:
- Alterations in the level of consciousness, smoking, hypoxemia, acidosis, toxic inhalations, pulmonary edema, uremia, malnutrition, immunosuppression, mechanical obstruction of a bronchus, elderly, cystic fibrosis, bronchiectasis, chronic obstructive pulmonary disease (COPD), alcoholism, seizure disorder
- HIV infection: 40-fold increase in risk
- Risk factors for HAP, VAP, HCAP:
- Intubation: 6- to 21-fold increase in risk
- If >70 years of age: COPD, depressed consciousness, aspiration, chest surgery, the presence of an intracranial pressure monitor or nasogastric tube, H2 blockers or antacid therapy, transport from the ICU for diagnostic or therapeutics procedures, previous antibiotic exposure (particularly to 3rd-generation cephalosporin), reintubation, hospitalization during fall or winter season, mechanical ventilation for acute respiratory distress syndrome (ARDS)
History Pneumonia
- Thick, yellow-green, bloody or rusty sputum
- Mental status changes: Anxiety, confusion, restlessness, obtundation, coma
- Abdominal pain, anorexia, diarrhea
- Cough, fever, dyspnea, chills
- Chest pain (pleuritic or nonpleuritic)
- Atypical:
- Insidious onset of dry cough
- Extrapulmonary symptoms: Diarrhea, headache, myalgias, sore throat
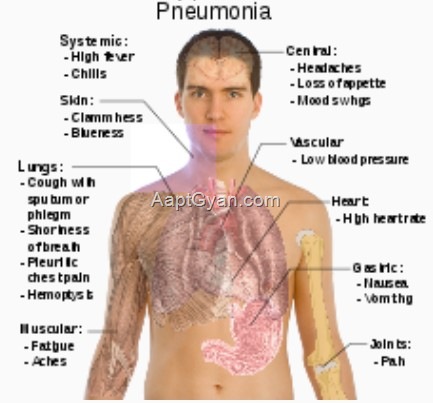
Symptoms of pneumonia
- Fever
- Chills
- Cough .
- Pleuritic chest pain
- Sputum production
- Body may be ,cold or hot. ,
Signs of pneumonia
- Fever
- Respiratory rate increased
- Dullness on percussion of lungs
- Bronchial breathing
- Aegophony
- Crackles and wheezes (crepts and ronchi) Pleural friction rub.
Pneumonia Physical Exam
- Pulse oximetry to evaluate oxygenation
- Tachypnea, tachy/bradycardia, cyanosis
- Decreased breath sounds, rales, friction rub
- Consolidation: Egophony, increased fremitus, pectoriloquy, dullness to percussion
- Abdominal tenderness or pain
- VAP is suspected when a patient receiving mechanical ventilation develops a new or progressive infiltrate with fever, leukocytosis, or purulent tracheobronchial secretions; increased respiratory rate, increased minute ventilation, decreased tidal volume, decreased oxygenation, or a need for more ventilator support or inspired oxygen
Chest X-ray of pneumonia
- One or more opaque patches in lung fields.
- Pneumonia may be Community-acquired – Serious, less serious.
- Hospital acquired – Patient on ventilator, Patient not on ventilator.
Routes of Infection for pneumonia
- Aspiration
- Droplet infection
- Hematogenous spread
- Direct spread of Infection.
- In healthy persons Streptococcus pneumoniae and Hemophilus influenzae are normally present in oropharynx.
- These can cause pneumonia during stress, surgery, low immune status.
- Aspiration pneumonia can occur post-operatively, during seizures in patients of strokes, in unconscious patients.
- Hematogenous spread occurs in
- Endocarditis
- IV catheter
- Infective conditions
- UTI.
- Common organism in such cases is Staphylococcus aureus.
- E.coli infection occurs from urinary tract.
- Aerosol infection is by M. tuberculosis, fungi, histolasma, legionella, Coxiella burneti, Influenza A and’ B.
Pathophysiology of pneumonia
- Vital capacity, lung compliance, functional residual capacity, total lung capacity are decreased.
- There is hypoxaemia. The pathological picture of lung shows:
- Lobar pneumonia
- Route of infection: Gross aspiration, microaspiration, aerosolization, hematogenous and direct spread
- Bronchopneumonia: Patchy consolidation involving one or several lobes
- Interstitial pneumonia: Interstitium, including alveolar walls and the connective tissue
- Vital capacity, lung compliance, functional residual capacity, and total lung capacity are below normal in patients with pneumonia. V/Q mismatch and intrapulmonary shunting are responsible for the hypoxemia.
Lobar pneumonia:
- Entire lobe involvement
Miliary pneumonia:
- Diffusely distributed 2- to 3-mm lesions (bloodstream spread)
- Bronchopneumonia
- Interstitial pneumonia
- Miliary pneumonia.
- Lobar Pneumonia
- One entire lug lobe is involved.
- There is homogenous opacity of one whole lobe seen on X-ray.
First stage:
- Congestion in first 24 hours.
- Bacteria, edema fluid and neutrophils invade the lung.
Second stage :
- It is red hepatiz.ation (so-called because the lungs resemble the colour and consistency of liver).
Third stage:
- is gray hepatization due to fibrino-purulent exudates and hemosiderin.
- This occurs by the 6th day.
Fourth stage or Final stage:
- is resolution,when pulmonary architecture is restored.
- There may be pleural adhesions also.
Bronchopneumonia
- Is a patchy consolidation involving one or several lobes, usually lower and posterior portions because of aspiration of oropharyngeal contents by gravity.
Interstitial pneumonia
- Involves the interstitial, alveolar walls, and connective tissue around the bronchovascular tree. Lesions are patchy or diffuse.
Miliary pneumonia
- There are 2 – 3 mm size lesions due to spread of ~acteria to lungs via blood stream.
- Causes of Miliary pneumonia are:
- Tuberculosis
- Histoplamosis
- Coccidioidomycosis
- Herpes
- Cytomegalovirus.
- Sometimes the patient is severely immunocompromized.
COMPLICATIONS OF PNEUMONIA
- Necrotizing pneumonia
- Lung abscess
- Lung infarction
- Cavitation
- Empyema
- Broncho-pleural fistula
- Interstitial emphysema
- Pneumothorax
- ARDS
- Lung fibrosis
- Pleural adhesions.