Article Contents ::
- 1 Glomerular Diseases
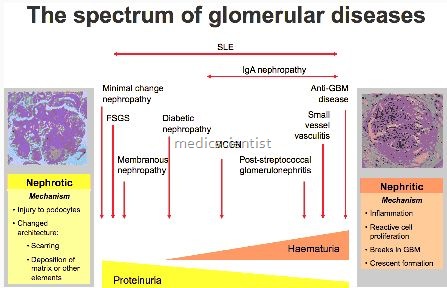
- 2 Some Type of Glomerular Diseases —
- 3 CLINICAL PRESENTATION OF GLOMERULAR DISEASE —
- 4 TYPES OF GLOMERULAR DISEASES Diffuse proliferative glomerulonephritis
- 5 Treatment
- 6 Crescentric GN (CGN) or Rapidly Progressive GN (RPGN)
- 7 Treatment
- 8 Focal proliferative GN
- 9 Treatment
- 10 Mesangioproliferative GN
- 11 Membrano proliferative GN
- 12 Minimal change GN
- 13 Focal segmental glomerulosclerosis
- 14 Nodular or global sclerosis
- 15 Treatment
- 16 Membranous GN
- 17 Treatment
- 18 Deposttlon diseases
- 19 Treatment
- 20 Thrombotic microangiopathy
- 21 Treatment
- 22 Non-immune basement membrane abnormalities
- 23 Waldenstrom’s Macroglobulinemia
- 24 Drugs which may cause Glomerulopathy Minimal change disease –
- 25 Membranous nep.hropathy –
Glomerular Diseases
- The glomerulus is a modified capillary network which delivers an ultrafiltrate to Bowman’s space. The Bowman space continues as the renal tubule. The glpmerular filtration rate or GFR is dependent on glomerular blood flow and ultrafiltration pressure and filtration surface i.e. mesangial cells.
- Glomerulonephritis or glomerulopathy means glomerular injury with inflammation and antibody deposition and complement activation.
- Glomerular diseases may be primary i.e. diseases of the kidney, or secondary, when it is part of a multisystem disorder.
- Primary glomerular diseases are due to kidney disease itself but systemic features like uremic syndrome, hypertension, pulmonary oedema etc. are due to glomerular dysfunction .
- The presence of some form of glomerular disease, as opposed to primary tubulointerstitial or vascular disease, is usually suspected from the history and from one or more of the following urinary findings
- Glomerular disease may be acute – over days or
- weeks, subacute or rapidly progressive – over weeks or months, or chronic – over months and years.
- Glomerular lesions may be focal or diffuse.
Some Type of Glomerular Diseases —
- Focal glomerular disease
- involves less than 50% of glomeruli.
- Diffuse glomerular disease
- involves more than 50% of glomeruli.
- Glomerular disease may be segmental or global
- depending on whether the glomerular tuft is involved partially or wholly.
- Membranous glomerulonephritis
- means deposition of immune substances on the glomerular basement membrane.
- Glomerulosclerosis
- means increase of extracellular material in GBM(glomerular basement memb::ane) and mesangium.
- Glomerular fibrosis
- means deposition of collagen due to healing of crescents resulting in tubulo–interstitial disease.
- Proliferative disease
- may be true proliferation of glom ruli or hypercellularity due to infiltration of leukocytes
- Endocapifiaty or intracapillary disease
- means mesangial cells”are involved.
- Crescentric glomerular disease
- is a half-moon shaped collection of cells in Bowman’s space.
- It is also called rapidly progressive glomerulo-nephritis because of its rapid course.
CLINICAL PRESENTATION OF GLOMERULAR DISEASE —
- Although there are many causes of glomerular disease, the patient’s age and the characteristics of the urine sediment usually allow the differential diagnosis to be narrowed prior to renal biopsy.
TYPES OF GLOMERULAR DISEASES Diffuse proliferative glomerulonephritis
- There is acute nephritic syndrome – red blood cells, RBC casts, leukocytes, subnephrotic proteinuria <3 g in 24 hours.
- There is acute renal failure over days to weeks with hypertension, edema, oliguria, active urine sediments, subnephrotic proteinuria.
Etiology —
- Idiopathic, immune complex GN, post infectious, SLE, . infective endocarditis, cryoglobulinaemia.
Treatment
- Antibiotics, Supportive therapy, Diuretics and antihypertensives, Dialysis.
- Prognosis is good in post-streptococcal GN-resolution occurs in 6-8 weeks.
- There may be proteinuria for 1 year or more.
- In SLE – treatment of lupus nephritis after renal biopsy.
- For extrarenal manifestations in SLE- give glucocorticoids, salicylates, antimalarials, cyclophosphamide.
Crescentric GN (CGN) or Rapidly Progressive GN (RPGN)
- There is subacute renal failure over weeks to months, active urine sediment, hypertension, edema, oliguria and proteinuria.
Etiology
- Immune complexes, Wegener’s granulomatosis, polyarteritis nodosa.
Treatment
- Glucocorticoids, Cyclophosphamide, by pulse IV therapy, or orally, followed by maintenance doses for 6 months or more.
- Plasmapheresis, dialysis, renal transplantation.
Focal proliferative GN
- There is mild to moderate glomerular infiltration.
- There is active urinary sediment and mild decline in GFR.
Etiology
- All ,the diseases which cause diffuse proliferative or RPGN can cause focal proliferative GN, IgA nephropathy.
Treatment
- Spontaneous remission does not occur.
- Glucocorticoids for 8 weeks may cause decrease in proteinuria.
- Glucocorticoids is given for 24 weeks.
- Cyclophosphamide and Cyclosporin may be given.
- Renal transplantation is the ultimate treatment.
Mesangioproliferative GN
- There is chronic glomerular inflammation with proteinuria, hematuria and hypertension with decrease i’fl GFR.
E‘tiology
- IgA nephropathy and all the diseases which cause diffuse proliferative and RPGN.
Treatment
- Immunosuppressive drugs, dialysis and renal transplant.
Membrano proliferative GN
- There is nephritic- and nephrotic picture, decline in GFR, active urine s’ediment, and proteinuria in nephrotic range.
Etiology
- Immune complex, thrombotic microangiopathies, deposition diseases, post renal or marrow transplantation.
Minimal change GN
- It is a common renal disease in children.
- It is also called nil disease, lipoid nephrosis, foot process disease. Glomerular size and architecture are normal.
- Presentation is nephrotic syndrome with proteinuria more than 3.5 gjday, hypoalbuminemia, edema, hyperlipidemia, thrombotic diathesis and decline in GFR upto 30%.
- There is benign urinary sediment.
- There may be microscopic hematuria. Hypertension is rare.
Etiology
- Idiopathic, drug-induced, HIV, interstitial nephritis, Hodgkin’s disease, other lymphomas.
Treatment
- It is highly steroid-responsive, prognosis is excellent.
- Steroids are given for 20 – 24 wks, 1-1.5 mgjkg body weight j day for 4 wks, followed by 1 mg jkg j day on alternate days for 4 wks.
- Treatment may be given up to 6 months. Relapse may occur.
- Cyclosporin, azathioprine may also be given especially in steroid-resistant cases.
Focal segmental glomerulosclerosis
- There is nephrotic syndrome
Etiology
- Idiopathic, secondary response to nephron injury.
Treatment
- Treat nephrotic syndrome
Nodular or global sclerosis
- There is proteinuria and chronic renal failure
Etiology
- Diabetic nephropathy and other glomerulopathies.
- Nephropathy occurs in 30% of type I DM and 20% of type II DM,
- Among patients of ESRD, type II DM is a very common cause because of the high incidence of type II DM worldwide.
- The risk factors for diabetic nephropathy are hypergIycemia, hypertension, proteinuria, cigarette smoking, hyperlipidemia.
Treatment
- Control of blood sugar:
- Control of hypertension ACE inhibitors
- ARBs (Angiotensin receptor blocker)
- Peritoneal dialysis, hemodialysis, renal transplantation.
Membranous GN
- There is nephrotic syndrome,
Etiology “,
- Idiopathic, infections-hepatitis Band C, Malarra, Leprosy, Schistomiasis, drugs (gold, Captopr:il5, autoimmune diseases-SLE, Rheumatuid arthritis, Paraneoplastic diseases.
Treatment
- Management of nephrotic syndrome, steroids, cyclophosphamide, cyclosporine, chlorambucil.
- Renal transplant is the ultimate treatment.
Deposttlon diseases
- There”is nephritic and nephrotic presentation with renal failure over the years.
Etiology
- Amyloid, cryoglobulinemia.
Treatment
- Colchicine, melphalan, prednisolone, stem cell transplantation.
Thrombotic microangiopathy
- There is renal failure (usually acute), hypertension, proteinuria. Urine contains RBCs.
Etiolgy
- Idiopathic, GI infections, cyclosporine, SLE, scleroderma, toxaemia, malignant hypertension.
Treatment
- Treat etiology and mange renal failure.
Non-immune basement membrane abnormalities
- There is hematuria and renal failure.
Etiogy Alport‘s syndrome –
- Hereditary nephritis, mesangial hypercellularity, focal and segmental glomerulosclerosis, damage of GBM (Glomerular Basement Membrane), progresses to ESRD.
- Treatment of Alport’s syndrome is ACE inhibitors, dialysis, transplantation.
- Nail-patella~yndrome – Hereditary autosomal dominant disorder, multiple bony abnormalities of elbows, knees, nail dysplasia, GBM thickening, interstitial fibrosis, glomerular sclerosis.
- The disease manifests with hematuria, proteinuria. Progression to ESRD in some cases.
Waldenstrom’s Macroglobulinemia
- Disease of IgM-secreting plasma cells, with decreased GFR and renal amyloidosis.
IgA nephropathy (Berger’s disease)
- It is a very common nephropathy – glomerulopdthy, with idiopathic etiology like Henoch-Schonlein purpura.
- It is found in association with chronic liver disease, idiopathic pneumonia, ankylosing spondylitis, Sjogren’s syndrome.
Sickle cell disease
- It is a hereditary glomerular disease seen with focal segmental glomerulosclerosis in homozygotes for sickle cell disease.
- There is anaemia, proteinuria, hypertension, nephrotic syndrome.
Drugs which may cause Glomerulopathy Minimal change disease –
- NSAIDs, Rifampicin; Ampicillin
Membranous nep.hropathy –
- Gold, Mercury, Captopril, Penicillamine
Necrotizing glomerulonephritis –
- Ciprofloxacin Proliferative glomerulonephritis with vasculitis
- Sulphonamide, Thiazides, Allopurinol, Penicillin.
RPGN (Rapidly Progressive Glomerulonephritis)-
- Rifampicin, Warfarin, Penicillamine, Amoxycillin, Carbimazole.