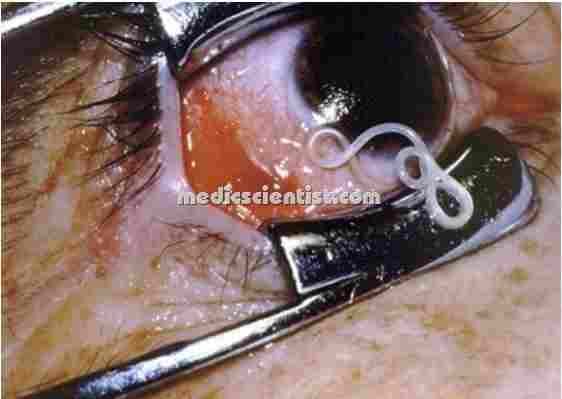
Filaria Nematode worm Disease of Lymphatic Systems Transmitted by Mosquitoes
Filariasis
- Massive swelling, esp. of the genitalia and lower extremities, resulting from obstruction of lymphatic vessels, for example by filarial parasites, malignancies, neurofibromatosis, or a familial congenital disease (Milroy’s disease).
- Prolonged swelling can cause an increase in interstitial fibrous tissue and skin puckering or breakdown. In patients with the filarial diseases
 |
|
Filaria Nematode worm Disease of Lymphatic Systems Transmitted by Mosquitoes
Filariasis
|
Filaria can occur due to three nematode worms.
- 1. Wuchereria bancrofti
- 2. Brugia malayi
- 3. Brugia timori.
 |
| Wuchereria bancrofti |
- All three infections are transmitted to man by the bite of mosquitoes.
- A parasitic worm that is the causative agent of elephantiasis.
- Adults of the species live in human lymph nodes and ducts.
- Females give birth to sheathed microfilariae, which remain in internal organs during the day but at night are in circulating blood, where they are sucked up by night-biting mosquitoes,
- Inside the mosquitoes microfilariae larva are continue their development, and becoming infective larvae in about 2 weeks
- All have similar life cycles with the adult worms living in the lymphatic vessels whilst the microfilaria circulate in peripheral blood.
 |
| Vector of Filaria Culex mosquito |
Vector of Filaria
- The microfilaria are taken in by the mosquito when they feed on the host.
- The vector for W. bancrofti is Culex mosquito.
- The vector for B. malayi is Mansonia mosquito. The vector for B. timori is Anopheles mosquito
- Filaria is transmitted by the bite of infected mosquito. The parasite is deposited at the site of puncture and passes through the skin and reaches the lymphatic system.
- The incubation period is 8 – 12 months or longer.
Clinical Features of FILARIASIS :
- · The disease may be asymptomatic or acute or chronic.
- · The important features are lymphangitis, lymphadenitis, elephantiasis of genitals, legs and arms.
- · It may also present as tropical pulmonary eosinophilia or filarial arthritis.
- · Filaria can cause great deformity and disability.
 |
| LYMPHATIC FILARIASIS |
LYMPHATIC FILARIASIS
- There may be no symptoms inspite of micro-filaria in the blood. The host acts as carrier.
- There may be recurrent episodes of acute inflammation in lymph nodes and lymphatics.
- There is periodic high grade fever, lymphangitis, lymphadenitis, lymphedema of various parts of body and even epididymoorchitis in males.
- The chronic stage may develop 10 years after the first attack. There is fibrosis and obstruction of lymphatic vessels causing permanent structural changes.
- There is hydrocele, elephantiasis and chyluria. Elephantiasis affects the legs, scrotum, arms, penis, vulva and breasts.
- Other causes of elephantiasis are tuberculosis, tumors, irradiation, silica poisoning.
 |
| OCCULT FILARIASIS |
OCCULT FILARIASIS
- There are no clinical manifestations of the parasite and microfilaria are not found in the blood e.g. tropical pulmonary eosinophilia.
Diagnosis of FILARIASIS:
- · A thick film made from capillary blood between 8.30 pm and 12.00 midnight is prepared on the glass slide and examined for microfilaria.
- · Membrane filter concentration (MFC) method is a sensitive method for detection of microfilaria.
- · Blood is collected from a vial and filtered to detect microfilaria.
- · DEC provocation test – Diethyl carbamazine (DEC) 100 mg is given orally to induce microfilaria to appear in blood within 15 minutes to 2 hrs.
- · Serological tests to detect antibodies to microfilaria using immunoflourescent and complement fixing techniques.
Treatment of FILARIASIS:
- Diethyl carbamazine (DEC) is safe and effective. 6 mg/kg body weight of DEC is given orally for 12 days in divided doses after meals.
- DEC kills the microfilaria. DEC can cause serious side effects like headache, nausea, vomiting and dizziness.
- Ivermectin is a broad spectrum macrolide antibiotic (microfilaricidal agent). It is given in doses of 200-400 µg/kg body weight.
- Other measures are control of vector by antilarval measures, removal of pistia plant and larvicidal (to kill the larvae) operation.
- DDT, HCH and Dieldrin can be sprayed. Pyrethrum is a new anti-vector spray.
