Heart Failure Treatment PHARMACOLOGICAL THERAPY
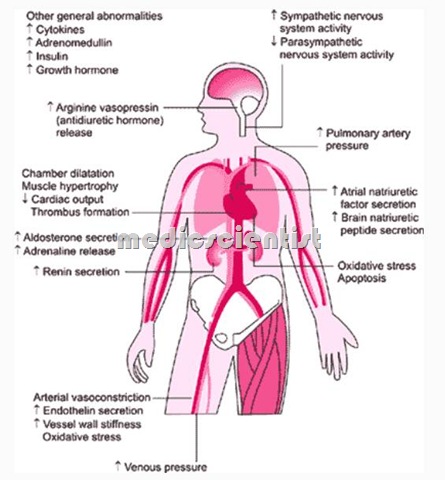
Heart failure (HF) is a common clinical syndrome representing the end-stage of a number of different cardiac diseases. Heart failure may result from arrhythmias, heart valve lesions,myocardial infarction, myocardial ischemia, congenital malformation of the heart or great vessels, pericarditis, cardiomyopathy, constrictive or conditions that affect the heart indirectly,

Heart Failure GENERAL PRINCIPLES —
- The management of HF begins with an accurate assessment of the etiology and severity of the disease
ACE Inhibitors (Angiotensin converting enzyme inhibitors) in Heart Failure
- · First line therapy of CHF
- · All cases with less than 40% LVEF (left ventricular ejection fraction)
- · Reduce risk of MI
- · Must be given after MI in any case
- · Improve systolic function
- · Prevent decompensation
- · Prevent sudden death
- · With or without symptoms
- · Uptitrated gradually to doses recommended
- · Relieve symptoms
- ·Improve functional capacity
Adverse effects of ACE Inhibitors –
- · Cough
- · Hypotension
- · Hyperkalemia
- · Angioedema
- · Renal insufficiency
- · Syncope.
Contraindications of ACE Inhibitors –
- · Pregnancy
- · Bilateral renal artery stenosis
- · Angioedema
- · Serum creatinine> 3.
Precautions with ACE Inhibitors –
- 1. Monitoring of renal function
- 2. Serum electrolytes monitored
- 3. Avoid potassium sparing diuretics
- 4. Avoid NSAIDs (Non steroidal anti-inflammatory drugs)
- 5. Avoid diuretics + vasodilators together.
Dose of ACE Inhibitors –
- Enalapril 10 mg BD
- Lisinopril 5 – 35 mg OD
- Captopril 50 mg TDS
- Ramipril 5mg BD.
ARBS (ANGIOTENSIN RECEPTOR BLOCKERS)
- · Alternative to ACE inhibitors
- · Same efficacy, Reduce mortality and morbidity
- · Can be combined with ACE inhibitors with caution
DIURETICS in Heart Failure
- · Loop diuretics
- · Thiazides
- · Metolazone.
- If GFR (glomerular filtration rate) <30 ml/min use loop diuretics
- metolazone is used for severe heart failure Potassium-sparing diuretics for hypokalemia
- High doses of diuretics used for fluid retention and dyspnoea.
BETA BLOCKERS – Why
- · For stable NYHA class II – IV
- Reduces morbidity
- · Improves function
- · Reduces mortality
Examples of Beta Blockers
- Atenolol
- Metoprolol
- Nebivolol
- · Bisoprolol
- · Carvedilol
ALDOSTERONE ANTAGONISTS in Heart Failure
- · They come after ACE Inhibitors, beta blockers, diuretics
- · Improves survival and morbidity
- · Useful after MI with LV systolic dysfunction
- · Useful in heart failure + diabetes
- · Exs are spirinolactone, eplerinone
- · Do not cause hypokalemia
CARDIAC GLVC:OSIDES should be given in Heart Failure
- · Heart failure
- · Heart failure + atrial fibrillation
- · Heart failure + tachycardia
- · Heart failure with/due to beta blockers
- · Reduces hospitalization
- · Very cheap
- ·Relieves symptoms.
Contraindications of digitalis in Heart Failure –
- · Bradycardia
- · 2nd and 3rd degree AV block
- · SSS (Sick Sinus Syndrome)
- · WPW syndrome
- · HOCM (Hypertrophic obstructive cardiomyopathy)
- · Hypokalemia
- · Hyperkalemia
- ·Carotid sinus syndrome.
Dosage of digitalis –
- · Daily dose 0.125 – 0.25 mg/day oral
- · IV dose 0.25 – 0.5 mg IV slowly for rapid digitalization
- · Serum creatinine should be monitored and dose reduced, if high.
VASODILATORS in Heart Failure
- · If ACE inhibitors or ARBs cannot be given:
- – Hydralazine
- – Nitrates
NESIRITIDE
- Recombinant human brain or B type natriuretic peptide (BNP) :
- Improves dyspnoea Causes vasodilatation Improves symptoms
- Hypotension may occur Clinical trials limited.
- Calcium sensitizer Prevents organ failure Improves symptoms Under trial.
ANTI-THROMBOTIC AGENTS in Heart Failure
- · In CHF (congestive heart failure) with AF (atrial fibrillation), thromboembolic events, LV thrombus, LA thrombus – antithrombotic agents strongly recommended
- After MI – Aspirin recommended
- Aspirin avoided in severe heart failure
- · Anticoagulant avoided in patients who cannot be monitored
- · In pure heart failure there is no beneficial effect.
ANTIARRHYTHMICS
- · Class I avoided (quinidine,procainamide)
- · Beta blockers recommended
- Amiodarone is given for AF (atrial fibnrillation)
- Amiodarone also given for ventricular
- arrhythmias
- · Amiodarone not used in pure heart failure.
OXYGEN THERAPY in Heart Failure
- • No special indication
SURGERY AND DEVICES in Heart Failure
- · Revascularization
- · Cardiomyoplasty
- · Batista procedure (repair of myocardium).
- · Mitral and aortic valve surgery if required
- · LV aneurysmectomy for ventricular aneurysm
- · Stem cell therapy
Pacemakers:
- Cardiac Resynchronization Therapy:
- CRT (Cardiac resynchronization therapy) Biventricular pacing in :
- Ventricular dyssynchrony QRS> 120 ms
- NYHA III – IV
- Severe symptoms
ICD (Implantable cardioverter defibrillator)
- · Indication for ICD is VT(ventricular tachycardia) or VF(ventricular fibrillation)
- · For NYHA class III – IV and LVEF <30%
- · ICD with CRT (cardiac resynchronization therapy) is the treament for severe heart failure
Heart transplant Indications :
- · For end-stage heart failure
- · For severe symptoms
- · If all therapy failed
- · If facilities available
- ·Donor heart needed. Contraindications :
- · Infection
- · Renal failure
- · Cancer
- · Pulmonary disease
- · Thromboembolism
- · Alcohol or drug abuse
- · Multiorgan disease.
Ventricular assist devices and Artificial heart
- · Useful for patients waiting for transplant
- · Acute myocarditis
- · For temporary hemodynamic support
- · Not for long term use
- · Not cost effective.
Ultrafiltration
- · For fluid overload refractory to diuretics
- · For severe heart failure
- · Temporary relief only.
Intraaortic balloon pumps used for
- · Severe heart failure
- · Cardiogenic shock.
Causes of refractory heart failure also called Worsening heart failure
- · Non compliance -Salt, Fluids, Lifestyle
- · Use of NSAIDs, Verapamil, Diltiazem
- · Infections
- · Alcohol and smoking
- · Renal failure
- · Pulmonary infarction
- · Anaemia
- , Heart block
- · MI (myocardial infarction)
- · Uncontrolled hypertension
- · Thyroid disease
- · Severe MR (Mitral regurgitation), TR (Tricuspid regurgitation).
- · Atrial fibrillation
- · SVT (supra ventricular tachycardia)
- · VT (Ventricular tachycardia)
- · Bradycardia
