Article Contents ::
All about Pheochromocytoma Clinical Features Diagnosis Treatment
Definition
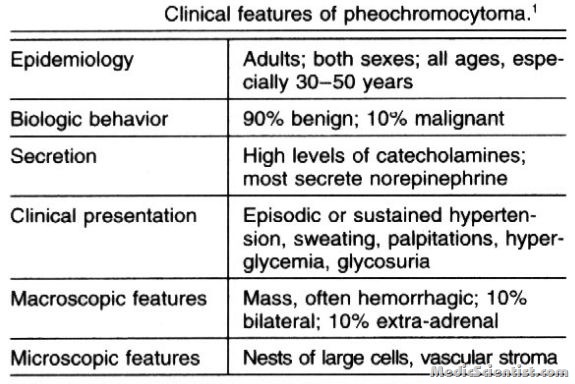
A tumor derived from neural crest cells of the sympathetic nervous system that is responsible for about 0.1% to 2% of all cases of hypertension. Catecholamine-secreting tumors that arise from chromaffin cells of the adrenal medulla and the sympathetic ganglia are referred to as “pheochromocytomas” and “extra-adrenal catecholamine-secreting paragangliomas” (“extra-adrenal pheochromocytomas”), respectively Pheochromocytomas are a group of cells which produce and secrete catecholamines. They are derived from adrenal medulla or chromaffin cells of the sympathetic ganglia. There is sinus tachycardia, bradycardia, supraventricular arrhythmias, ventricular premature contractions, angina and acute myocardial infarction.
CLINICAL PRESENTATION —
- The most common feature of pheochromocytoma is hypertension and paroxysmal hypertension which may be very disturbing.
- It is a correctable cause of hypertension.
- Untreated pheochromocytomas may be fatal. Pheochromocytomas are situated in the adrenal medulla or in abdomen near the celiac, superior mesenteric and inferior mesenteric ganglia (sympathetic ganglia).
- It occurs at all ages but common in young age. It is more common in females.
- There is labile hypertension, seizure disorders, anxiety attacks. Sometimes it is detected during surgery or after trauma.
- There is headache, excessive sweating and palpitations.
- There may be pain in chest and abdomen, with nausea and vomiting.
- There may be sudden flushing.
- Pheochromocytoma is usually suggested by the history in a symptomatic patient, discovery of an incidental adrenal mass, or the family history in a patient with familial disease.
Diagnosis
- The patient’s urine or blood is tested to determine whether it contains excessive levels of catecholamines or their metabolites.
- · Vanillylmandelic acid, metanephrines, unconjugated and free catecholamines are estimated in urine.
- · Plasma catecholamines and plasma metanephrines may be measured for diagnosis.
When to suspect pheochromocytoma —
- Hyperadrenergic spells (eg, self-limited episodes of nonexertional palpitations, diaphoresis, headache, tremor, or pallor)
- Resistant hypertension
- A familial syndrome that predisposes to catecholamine-secreting tumors (eg, MEN2, NF1, VHL)
- A family history of pheochromocytoma
- An incidentally discovered adrenal mass Hypertension and diabetes Pressor response during anesthesia, surgery, or angiography Onset of hypertension at a young age (eg, <20 years)
- Idiopathic dilated cardiomyopathy
- A history of gastric stromal tumor or pulmonary chondromas (Carney triad)
Treatment Pheochromocytoma
- Phenoxybenzamine, an alpha receptor blocker, in dose of 10 mg 12 hourly, increasing 10 mg every few days, till blood pressure is controlled and paroxysms disappear.
- For tachycardia, after alpha blockers, beta blockers may be given in low dose.
- The tumors may be localized by eT, MRI and removed surgically.
- Once a pheochromocytoma is diagnosed, all patients should be operated on after appropriate medical preparation.
- Extirpating a pheochromocytoma is a high-risk surgical procedure, and an experienced surgeon/anesthesiologist team is required.
