Rheumatic Fever Signs and symptoms Diagnosis of Rheumatic fever Causes with treatment —
Rheumatic fever is acute or first presentation of infection by Streptococcus leading to sore throat, fever, arthritis and/or carditis. A multisystem, febrile inflammatory disease that is a delayed complication of untreated group A streptococcal pharyngitis. Pharyngitis usually occurs two to four weeks before the onset of ARF symptoms. Rheumatic heart disease refers to a chronic rheumatic infection leading to irreversible, permanent damage of heart valves.
Rheumatic Fever Etiology
- Rheumatic fever is caused by group A beta hemolytic streptococcal infection.
- The disease starts with upper respiratory tractinfection-streptococcal sore throat. After a gap of a few months to a few years involvement of the heart ocurs in the form of valvular heart diseas,.
Age
- Can occur at any age but typically occurs from 5 to 15 year.
Rheumatic Fever Epidemiology
- Rheumatic fever is more common in :
- Families of affected individuals
- Poor housing conditions
- Poor (low socioeconomic status) people
- Overcrowding.
Rheumatic Fever Pathogenesis
- The pathogenic mechanisms that lead to the development of acute rheumatic fever remain incompletely understood.
- After streptococcal infection of the throat, the development of rheumatic fever depends upon the immunity of the host, the virulence of the bacteria, individual resistance, serotype 1,3,5,6,18, abnormal immune response of the host, unique surface markers on non T lymphocytes.
- molecular mimicry is thought to play an important role in the initiation of the tissue injury
- The ‘oints and heart valves are involved in Rheumatic fever and Rheumatic heart disease by :
- 1. Direct infection
- 2. Toxic effect of extra-cellular products of bacteria
- 3. Abnormal immune response
- The theory of antigenic mimicry for rheumatic fever means that some antigens of the streptococci are similar to the host tissues and hence are destroyed by the antibodies produced by the host.
Diagnosis of Rheumatic fever
- The diagnosis of rheumatic fever cannot be determined readily by laboratory tests,
- the approach to such patients, and to children with initially unexplained fever are presented separately.
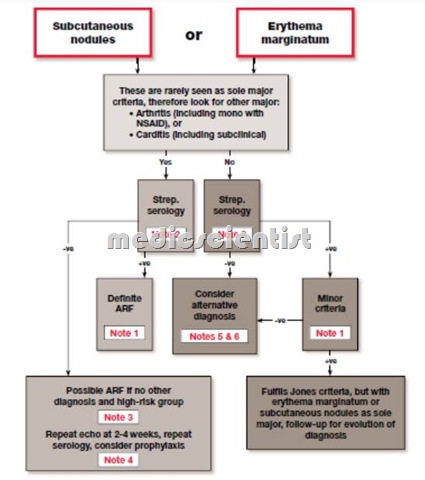
- Rheumatic fever is diagnosed by application of Jones criteria updated in 1992.
- There are 5 major criteria and few minor criteria plus supporting evidence of streptococcal infection.
- As an example, serial chest radiographs may be helpful in following the course of carditis,
Rheumatic Fever Major criteria
- 1. Carditis
- 2. Arthritis
- 3. Chorea
- 4. Subcutaneous nodues
- 5. Erythema marginatum.
Rheumatic Fever Minor criteria
- 1. Fever
- 2. Arthralgia
- 3. Increased ESR
- 4. Increased C-reactive protein
- 5. Increased PR interval
- 6. History of rheumatic fever and history of sore throat.
Essential evidence
- · Positive throat culture for group A streptococcus.
- · Positive Rapid antigen detection tests.
- · Elevated streptococcal antibody titer-ASO titer (Anti-Streptolysin 0).
MAJOR CRITERIA
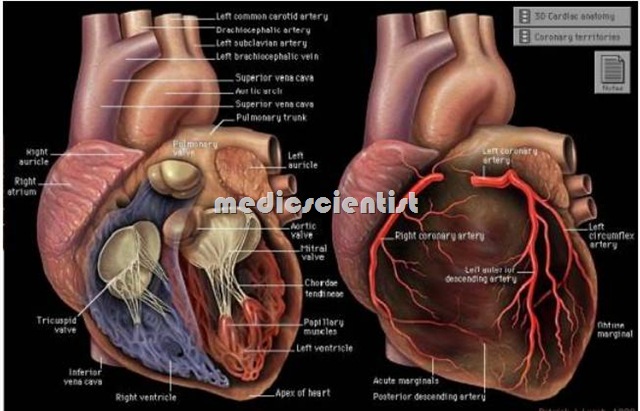
Carditis
- There is pancarditis Le. pericarditis, myocarditis, endocarditis.
Pericarditis:
- There is very little serous effusion like butter on bread (bread and butter appearance) and no constriction, pericardial friction rub.
Endocarditis:
- There is inflammation of heart valves leading to murmur of mitral stenosis (Care’s Coomb’s murmur-blowin mid-diastolic murmur at the a ex murmur of aortic regurgitation, and mitral regurgitation.
Myocarditis:
- There is sinus tachycardia, mitral regurgitation, S3 gallop, MR, TR, increased PR interval, heart failure.
Arthritis
- The arthritis lasts for a few days in one joint and then occurs in another joint, even before it is cured in the first joint.
- When the joint is cured, there is no sequelae or residual deformity of the joint.
- Arthritis is migratory, affecting the ankles, wrists, knees, and elbows.
- Usually the small joints of the hand and feet are not involved.
- Big joints like hip joints are not involved.
- Typically the arthritis lasts for a day or two in one joint. It flits from one joint to another. This migrating polyarthritis lasts for a few days to weeks affecting one or two joints at a time.
- The pain of rheumatic arthritis responds dramatically to 2 g of aspirin given 4 times a day (3-4 tablets given 4-6 hou rly).
Chorea
- In children the chorea starts with restlessness, change in handwriting, irritability, and later typical movements of the trunk and whole body.
- Rheumatic chorea is called Sydenham‘s chorea or St. Vitus Dance.
- It occurs several months after the streptococcal infection. It is very rare.
Subcutaneous nodules
- These are small and found over extensor surface of joints in long-standing Rheumatic heart disease (RHD). They may disappear in few days.
Erythema marginatum
- These are transient macular eruptions with rounded borders, may be with irregular margins, specially on the trunk, pink in color, non pruritic (do not itch).
- they are very uncommon in Indians.

EVIDENCE OF STREPTOCOCCAL INFECTION
- he organism-beta hemolytic streptococcus may be grown on culture from throat swabs-2 or 3 cultures ay be done.
- Rapid antigen test for streptococcus may be done. Group A streptococcal antibodies may be measured i.e. Antistreptolysin 0 (ASO) – more than 200 units, anti-deoxyribonuclease B (antiDNAse-B), anti hyaluronidase, antistreptozyme test (ASZ).
- At least 80% of ARF patients will have raised ASO.
Rheumatic Fever Diagnosis
CLINICAL MANIFESTATIONS —
- Acute rheumatic fever occurs most frequently in children from four to nine years of age.
- Rheumatic fever is diagnosed by application of lanes criteria updated in 1992.
- There a’re 5 major criteria and few minor criteria plus supporting evidence of streptococcal infection.
- The onset of the disease usually is characterized by an acute febrile illness that may manifest itself in one of several ways:
- Migratory arthritis predominantly involving the large joints Carditis and valvulitis Central nervous system involvement (eg, Sydenham chorea) Rash Some combination of the above
- At least 2 major or 1 major and 2 minor criteria plus essential evidence of streptococcal infection is required to diagnose rheumatic fever.
- · Usually arthritis and carditis do not occur together.
- · Subcutaneous nodules and erythema marginatum are usually not present at initial diagnosis.
- · Presence of multiple features of Jones criteria indicate active disease.
- · Patients of RF may present with chronic valvular heart disease but without history of rheumatic arthritis.
- · Patients of rheumatic chorea usually have no arthritis or carditis.
Treatment of Rheumatic fever
- Treatment of acute rheumatic fever consists of antibiotic therapy, heart failure management, and anti-inflammatory therapy.
- Antistreptococcal antibiotics Treatment of clinical manifestations Prophylaxis of RF.
- Prevention of initial and recurrent attacks of rheumatic fever depends on control of group A streptococcal tonsillopharyngitis
Antistreptococcal antibiotics
- Oral penicillin V 500 mg BD for 10 days.
- If allergic to penicillin then erythromycin 250 mg 4 times daily for 10 days.
- Or intramuscular bel1zathine penicillin G single crose-single intramuscular injection of 1.2 mllion units, after sensitivity tes.
Treatment of Clinical manifestations
Arthritis:
- Prednisone should be avoided as anti-inflammatory
- Salicylates 2 g 4 times daily Otlier analgesics also give relief
- Duration of anti-inflammatory drugs should be 4-6 wks and then gradually tapered till ESR returns to normal.
Carditis:
- Bed rest at least for a few days is advised to all patient of carditis and patients of arthritis.
- Salicylates and prednisone may have some antiinflammatory effect.
- Digitalis, Diuretics, ACE inhibitors may be used for LV dysfunction and heart failure.
Chorea:
- Diazepam, phenothiazines, phenobarbitone may be given for chorea.
PROPHYLAXIS FOR RHEUMATIC FEVER
- Prophylaxis consists of benzathine penicillin 1.2 million units (12 lacs) intramuscular after sensitivity test every 21 days.
- If the patient is allergic to penicillin then erythromycin 250 mg BD or Sulphadiazine 1 g daily is given for 5 years.
- Patients who have had an attack of rheumatic fever are very prone to recurrence. Each attack of rheumatic fever leads to increasing damage to the heart
- valves. Therefore all patients of rheumatic fever must be given prophylaxis for at least 5 years or more from last attack.
Antibiotic therapy for Rheumatic Fever Treatment —-
| Adults and adolescents (>27 kg or 60 lb) | Children (27 kg or 60 lb) |
| Oral penicillin V* | |
| 500 mg two to three times daily for 10 days | 250 mg two to three times daily for 10 days |
| Intramuscular penicillin (Bicillin C-R); single dose | |
| Benzathine penicillin G 900,000 unitsmixed with Procaine penicillin G 300,000 units | Benzathine penicillin G 900,000 unitsmixed with Procaine penicillin G 300,000 units |
| Amoxicillin | |
| 875 mg orally twice daily or 500 mg three times daily for 10 days | 40 mg/kg per day orally in two or three equally divided doses for 10 days |
| Cephalexin | |
| 500 mg orally twice daily for 10 days | 25-50 mg/kg per day orally in two equally divided doses(maximum 1000 mg per day) for 10 days |
| Azithromycin | |
| 500 mg orally on day one followed by 250 mg daily on days two through five | 12 mg/kg orally once daily for five days |
| Clindamycin | |
| 600 mg/day orally in two to four equally divided doses for 10 days | 20 mg/kg per day orally in three equally divided doses for 10 days |
