Article Contents ::
- 1 Lymphoid Malignancies Arise from cells of immune systems. and HODGKIN’S DISEASE
- 2 Lympho’ malignancy is may present as —
- 3 lymphoid disorders —
- 4 Immunological classification of Acute Leukemias :
- 5 Lymphoid Malignancies Etiology Leukemias
- 6 Chronic lymphoid leukemia (Cll)
- 7 Acute lymphoid leukemia (All)
- 8 L3 or Burkitts lymphoma/leukemia
- 9 T-cell lymphomas
- 10 Immunology
- 11 Lymphoid Malignancies Genetic Factors Leukemias
- 12 Specific genetic abnormalities have not been identified for most lymphomas. Prognosis
- 13 Lymphoid Malignancies Treatment for Leukemias
- 14 B cell chronic lymphoid leukemia / small lymphocytic lymphoma
- 15 HODGKIN’S DISEASE
- 16 Rye’s classification of Hodgkin’s disease
- 17 1. Classic Hodgkin‘s disease is of four types:
- 18 i. lymphocytic predominance
- 19 II. Nodular lymphocytic predominant Hodgkin‘s disease.
- 20 Diagnosis is by biopsy
- 21 The Ann Arbor staging system for Hodgkin’s Disease:
- 22 Treatment of HODGKIN’S DISEASE
Lymphoid Malignancies Arise from cells of immune systems. and HODGKIN’S DISEASE
Lymphoid Malignancies Arise from cells of immune systems, Immunological classification of Acute Leukemias , Acute lymphoid leukemia (All) , 8 cell ALL is the most common cancer in childhood. Incidence of ALL and AML increases in elderly Children with Down’s syndrome (trisomy 21) have increased risk of ALL and AML (acute myeloid leukemia) is more common in children and young adults. Childhood ALL is more common in high socioeconomic groups.
 |
| Lymphoid Malignancies |
Lymphoid Malignancies Arise from cells of immune systems.
Lympho’ malignancy is may present as —
- · Leukemia – involvement of bone marrow and blood.
- ·Lymphomas – solid tumors of immune systems. A patient of lymphoma may develop manifestation of leukemia later in life.
lymphoid disorders —
- that can present as chronic leukemia are:
- · Follicular lymphoma
- · Mantle cell lymphoma
- · Hairy cell leukemia
- · Adult T cell leukemia
- · Sezary syndrome.
- Chronic leukemias may be of lymphoid or myeloid origin.
- Acute leukemias are malignancies of blast cells of myeloid type or lymphoid types.
- French-American-British (FAB) Group divided Iymphomalignanc is of :
- · Small uniform blasts – L1 (typical childhood acute lymphoblastic leukemia.
- · Larger variable size cells – L2.
- · Uniform cells with basophilic vacuolated cytoplasm – L3 (Burkitts lymphoma).
Immunological classification of Acute Leukemias :
- · T cell
- · B cell
Lymphoid Malignancies Etiology Leukemias
 |
| Lymphoid Malignancies Etiology of Leukemias |
Chronic lymphoid leukemia (Cll)
- is frequent in adults, rare in children. More common in men and whites. Etiology unknown.
Acute lymphoid leukemia (All)
- is more common in children and young adults. Childhood ALL is more common in high socioeconomic groups.
- Incidence of ALL and AML increases in elderly Children with Down’s syndrome (trisomy 21) have increased risk of ALL and AML (acute myeloid leukemia)
L3 or Burkitts lymphoma/leukemia
- more common in children
- Etiology – Epstein-Barr virus infection in infancy.
T-cell lymphomas
- are more common in Asians. High energy radiation in childhood increases risk of T cell acute lymphoblastic leukemia.
- Industrial exposures, exposure to agricultural chemicals and smoking increase risk of ALL in adults. Hodgkin’s disease
- is of B cell origin. More common in whites and males. More common at ages of 20s and 80s.
- Younger patients have nodular sclerosing type of Hodgkin’s. Elderly patients and patients with HIV have lymphocyte-depleted Hodgkin’s or mixed-cellularity Hodgkin’s.
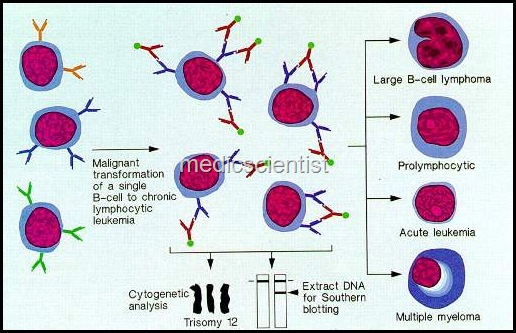
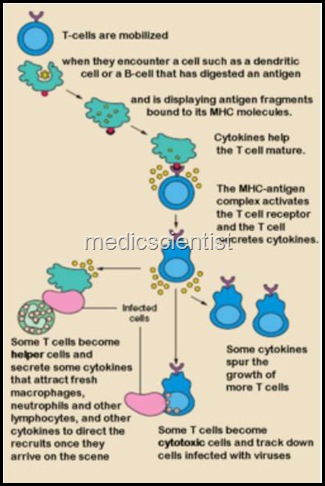
Immunology
- All lymphoid cells are derived from lymphoid, myeloid, erythroid, monocyte and megakaryocyte lineage.
- The cells may develop into lymphoid cells, T cells or B cells. Most lymphoid leukemias and lymphomas are of B cell origin. T cell differentiation occurs in thymus.
Lymphoid Malignancies Genetic Factors Leukemias
| Lymphoid Malignancies Genetic Factors |
Specific genetic abnormalities have not been identified for most lymphomas. Prognosis
Patients with blood and bone marrow showing leukemia, no lymphadenopathy, organomegaly, or signs of bone-marrow failure have good prognosis. Patients with lymphadenopathy, and organomegaly, have intermediate prognosis. Patients with bone marrow failure (hemoglobin less than 10 gm I dl or platelet count less than 100,00011l1) have bad prognosis.
- If bone marrow failure is due to autoimmune process or hypersplenism, then glucocorticoids and splenectomy are beneficial and improve the prognosis.
- Patients with B cell Cll may have autoimmune hemolytic anaemia, thrombocytopenia, and hypogammaglobulinemia.
- PRECURSOR CELL B CELL NEOPLASMS Precursor B cell lymphoblastic leukemia / lymphoma.
8 cell ALL is the most common cancer in childhood.
- The malignant cells are of B cell origin.
- There are signs of bone marrow failure such as pallor, fatigue, bleeding, fever and infections.
- There is anaemia, thrombocytopenia, leukopenia or leukocytosis.
- Extranodal sites may be involved in patients of leukemia like lymphadenopathy, hepatomegaly, splenomegaly, CNS disease.
- Diagnosis is by bone-marrow biopsy which shows infiltration by malignant Iymphoblasts.
Lymphoid Malignancies Treatment for Leukemias
- Induction of remission with combination chemotherapy, a consolidation phase and treatment for elimination of disease and then a period of continuing therapy till cure is achieved.
- The treatment is same as in any leukemia.
- The cure rate is high in disease of lymph nodes only.
B cell chronic lymphoid leukemia / small lymphocytic lymphoma
 |
| B cell chronic lymphoid leukemi |
- B cell Cll is the most common lymphoid leukemia and one of the common Non-Hodgkin’s lymphomas.
- Diagnosis is made when circulating lymphocytes are more than 4xl09/l, monoclonal B cells with CD 5 antigen.
- The peripheral blood smear shows smudge cells. This diagnosis must be considered in any patient with autoimmune hemolytic anemia or thrombocytopenia.
- Diagnosis can be made by lymph node biopsy.
- B cell Cll may be found accidentally on CBC examination, or when patient complains of fatigue, frequent infections or lymphadenopathy.
Treatment
- If patient has bone marrow involvement and lymphocytosis only, no specific therapy may be given.
- If the patient has lymphadenopathy, hepatosplenomegaly but no symptoms, then therapy may or may not be given.
- Patients who have bone marrow failure are serious and given specific antileukemia therapy.
- Glucocorticoid therapy and gamma globulins are given to patients with cytopenias and hypogamma globulinemias.
- The specific drugs are chlorambucil or fludarabine.
HODGKIN’S DISEASE
- Hodgkin’s disease is of B cell origin. It is more common in whites than black. It is more common in males than females. It may occur in the age group 20’s or 80’s.
- Patients in younger age groups have nodular sclerosing type of Hodgkin’s.
- HIV infected and elderly patients have mixed cellularity or lymphocyte-depleted Hodgkin’s disease.
- Reed-Sternberg giant cells or mirror-image giant cells are typically found in Hodgkin’s lymphoma.
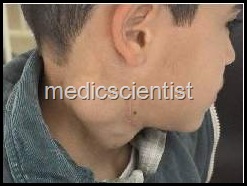
- There is palpable lymphadenopathy.
- The lymph nodes are non-tender, rubbery, discrete. Supraclavicular, axillary, cervical and mediastinal lymph nodes are enlarged.
- There may be enlargement of subdiaphragmatic lymph nodes in elderly. There is fever, night sweats, weight loss.
- The fever persists for days to weeks and then patient has no fever followed by recurrence of fever again. This is known as Pel-Epstein fever.
- There may be cerebellar degeneration, nephrotic syndrome, thrombocytopenia, and painful lymph nodes when patient takes alcohol.
Rye’s classification of Hodgkin’s disease
 |
| HODGKIN’S DISEASE |
1. Classic Hodgkin‘s disease is of four types:
i. lymphocytic predominance
- • the prognosis is excellent ii. Nodular sclerosis
- • prognosis is very good iii. Mixed cellularity
- • prognosis is good iv. lymphocytic depletion • poor prognosis
II. Nodular lymphocytic predominant Hodgkin‘s disease.
- · This may transform into B-cell NHl (Non
- Hodgkin’s lymphoma).
Diagnosis is by biopsy
- Majority have nodular sclerosing type of disease. For staging, a careful history, physical examination, CBC, ESR, lDH, chest X-ray, CT chest, CT abdomen, CT pelvis, bone marrow biopsy should be done.
- PET scan and Galium scan are very helpful in diagnosis.
The Ann Arbor staging system for Hodgkin’s Disease:
- Stage I: Involvement of single lymph node group or structure like spleen or thymus.
- Stage II : Involvement of 2 or more lymph node groups on same side of diaphragm.
- Stage III: Involvement of lymph node groups or structures on both sides of diaphragm.
- Stage IV :Involvement of extra nodal sites. Involvement of liver or bone marrow.
These stages are further divided into A, B or C.
- A – No symptoms
- B Unexplained weight loss> 10% of body weight in 6 months or fever more than 38°C
- C – Involvement of extra lymphatic tissue alone.
Treatment of HODGKIN’S DISEASE
- Chances of cure are more than 90%.
- Extended field radiotherapy has a high cure rate. After a brief course of chemotherapy, radiotherapy is given.
- Drugs used are Doxorubicin, Bleomycin, Vinblastine, Dacarbazine (ABVD).
- The MOPP regime consists of Mechlorethamine, Vincristine, Procarbazine and Prednisone.
- A weekly regimen for 12 weeks called Stanford V along with radiation therapy is being used in US.
- Another regime BEACOPP is also used in Europe. Autologous bone marrow transplantation is done for patients who fail in chemotherapy.
