All about Tuberculosis , EXTRA PULMONARY.Details about EXTRA PULMONARY TUBERCULOSIS Diagnosis Signs and Symptoms with Treatment.
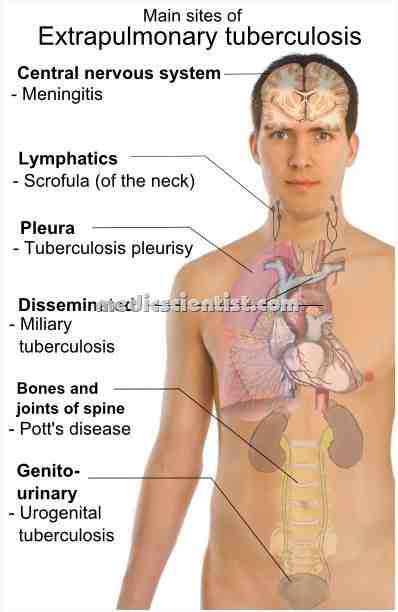
An infectious disease caused by the tubercle bacillus, Mycobacterium tuberculosis, and characterized pathologically by inflammatory infiltration, caseation, necrosis, abscesses, fibrosis,formation of tubercles, and calcification. The lungs are the major site for Mycobacterium tuberculosis infection. Pulmonary manifestations of tuberculosis (TB) include primary, reactivation, endobronchial, and lower lung field infection. It most commonly affects the respiratory system, but other parts of the body such as the gastrointestinal and bones, joints, nervous system, lymph nodes, genitourinary tracts, and skin may also become infected.
 |
| EXTRA PULMONARY TUBERCULOSIS |
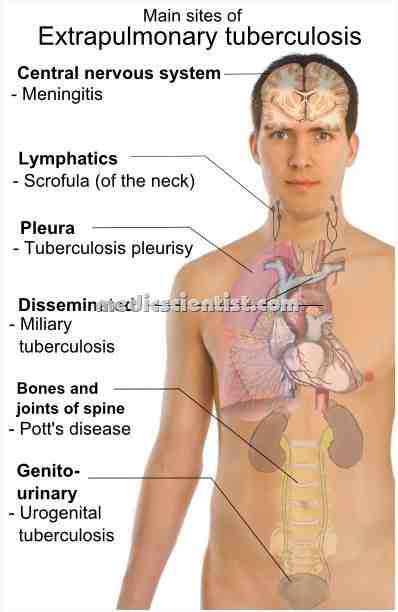 |
| EXTRA PULMONARY TUBERCULOSIS sites of involvemen |
- · Lymph nodes
- · Pleura
- · Genitourinary tract
- · Bones and joints
- · Meninges
- · Peritoneum
- · Pericardium
- · Any organ may be involved.
- Although the cervical region is most frequently involved, other sites are also described, Tuberculous infection of axillary, inguinal etc.
- The most common presentation is an isolated chronic nontender lymphadenopathy in a young adult patient without systemic symptoms.
- So it called tubercularIymphadenitis. Common in HIV positive patients.
- Tuberculous lymphadenitis, known centuries ago as the King’s evil and as scrofula when occurring in the cervical region, continues to be a common cause of extrapulmonary tuberculosis
- It is due to M. bovis and M. tuberculosis. Lymph node enlargement is painless.
- Common lymph nodes are cervical and supraclavicular.
- The enlargement around the neck is called scrofula. May be discrete(separate) but matted(adherent) later. A fistulous tract or sinus may be seen later draining caseous matter.
- Lung tuberculosis mayor may not be present.
- Fine needle aspiration biopsy confirms the diagnosis. AFB(acid fast bacilli) is present in 50% cases. Histology shows granulomatous lesion with caseation . DID is lymphoma and carcinoma.
- The human immunodeficiency virus (HIV) epidemic has been associated with an increase in the total incidence of TB and with an increased proportion of miliary, disseminated, and extrapulmonary TB
- For non-HIV infected patients, the occurrence of isolated peripheral (eg, cervical) , TB lymphadenopathy is very likely due to reactivation of disease at a site which was initially seeded by the hematogenous route during primary TB infection, perhaps years earlier
- When M tubereculosis penetrates the pleura, it results in pleural tuberculosis.
- Tuberculous pleural effusion accounts for approximately 5 percent of all disease due to Mycobacterium tuberculosis
- Pulmonary TB produces chronic cough, sputum production, fevers, sweats, and weight loss.
- The tuberculous pleural effusion is generally a self-limited effusion that can occur with either primary or reactivation disease.
- TB may also cause neurological disease (meningitis), bone infections, urinary bleeding, and other symptoms if it spreads to other organs.
- There is pleural effusion which may be minimal to massive.
|
| Signs and Symptoms EXTRA PULMONARY TUBERCULOSIS |
Signs and Symptoms EXTRA PULMONARY TUBERCULOSIS-
- There is fever, pleural pain, dyspnoea.
- TB may also cause neurological disease (meningitis), bone infections, urinary bleeding, and other symptoms if it spreads to other organs.
- uberculous pleural effusion is usually an acute febrile illness causing a nonproductive cough.
Physical findings
- Dullness on percussion V Absent breath sounds
- Pleural friction rub may be present Pleural effusion
- Pneumonia – Parenchymatous tuberculosis Thoracocentesis –
- Pleural fluid is straw coloured, may be haemorrhagic, exudate – protein more than 50% of serum value, low glucose, pH < 7.2, WBCs 500 – 2500 11-11, neutrophils or monocytes. AFBs not usually seen, culture is positive in lj3rd.
Needle biopsy – of pleura shows granulomas. Response to chemotherapy is good.
Tuberculous empyema:
- When a tubercular cavity in the lung ruptures, mycobateria enter pleural space. A broncho pleural fistula may also form.
X ray –
- shows pyopneumothorax with air fluid levels. Effusion is purulent and thick, containing lymphocytes.
- AFB (acid fast bacilli or mycobacteria) is seen in pleural fluid.
Treatment –
- is chemotherapy plus surgical drainage of fluid. Common complication is pleural fibrosis and restrictive lung disease.
|
| Tuberculosis of Upper airways |
- Larynx, pharynx, and epiglottis are involved.
- There is hoarseness, dysphagia, chronic cough with expectoration.
- AFB may be seen in sputum.
|
| Tuberculosis of Upper airways |
|
| Genitourinary tuberculosis |
- Involvement is by hematogenous spread. There is frequency, dysuria, hematuria, flank pain. Sometimes patient may be asymptomatic. There may be pyuria and hematuria.
- Hydronephrosis and renal damage may occur. Genital tuberculosis is more common in females in fallopian tubes and endometrium. It can cause infertility, pelvic pain and menstrual abnormalities.
- In males it can involve epididymis, with fistula, orchitis, prostatitis, UTI.
Investigations –
- Urine culture is negative.
- IVP (Intravenous pyelography) reveals calcification and details of ureteral structures.
- 3 morning urine samples must be cultured. Diagnosis – is by biopsy or culture of D & C (dilatation and curettage)products.
Chemotherapy –
- is given to all patients of genito urinary tuberculosis.
- Bone and joint infection may account for 10 to 35 percent of cases of extrapulmonary tuberculosis and, overall, for almost 2 percent of all cases of TB
- Spinal TB (Pott’s disease) most often affects the lumbar and lower thoracic region; upper thoracic and cervical disease is less common but potentially more disabling
- Infection comes from the blood or paravertebral lymph nodes.
- Spine, hips, and knees are involved.
- he next most common syndrome is tuberculous arthritis followed in frequency by extraspinal tuberculous osteomyelitis
- Spinal tuberculosis is also called Pott’s disease or tuberculous spondylitis. It involves two or more vertebra.
- In children, upper thoracic spine is involved.
- In adults, lower thoracic and upper lumbar vertebrae are affected.
- The intervertebral disc is also involved.
- There is collapse of vertebrae with kyphosis or gibbus.
- A paravertebral cold abscess may form Skeletal tuberculosis .
- In upper spine the abscess may reach upto chest wall. In lower spine it may reach inguinal ligaments or form a psoas abscess.
- CT and MRI show the details.
- Aspiration of abscess and biopsy of bone shows typical tubercular pathology.
- Pott’s spine leads to paraplegia due to an abscess or lesion compressing the spinal cord.
- An abscess causing paraplegia must be drained immediately.
- Skeletal tuberculosis , Tuberculosis of hip joints causes pain and limping. Tuberculosis of knee causes pain, swelling.
- Joints are gradually destroyed.
- Chemotherapy and surgery is required.
1. Tuberculosis suspect : Any person with symptoms or signs suggestive of tuberculosis like cough more than 2 weeks. 2. Case of tuberculosis: A patient in whom tuberculosis is confirmed bacteriologically 3. Definite case of tuberculosis : A patient with positive culture for M. tuberculosis complex or patient with 2 sputum smears showing AFB
History of treatment – Definitions for diagnosis:
- 1. New -A patient who has never taken antitubercular treatment or taken for less than a month.
- 2. Relapse -A patient treated for TB and declared cured, or full treatment taken but smear or culture for tuberculosis is positive.
- 3. Treatment after failure – A patient given An again, after failed previous treatment
- 4. Treatment after default – If a patient, bacteriologically positive, interrupts treatment for 2 moths or more and starts An again.
- 5. Transfer in – A patient transferred from another TB centre for continuation of treatment.
- 6. Other – Any other case like chronic case, sputum positive at the end of repeat treatment.
- Sometimes pulmonary and extra pulmonary relapse cases may be smear-negative.
RUGS – ATT (ANTITUBERCULAR TREATMENT)
- There are 3 main properties of antituberculous drugs:
- 1-Bactericidal action
- 2-Sterilizing activity
- 3-To prevent resistance.
Complete ANTITUBERCULAR TREATMENT