Article Contents ::
HYPEREOSINOPHILIC SYNDROME
Differential History ,Diagnosis ,Pathophysiology ,Treatment Of HYPEREOSINOPHILIC SYNDROME
- A persistently elevated eosinophil count >1,500 cells/µL for at least 6 months
- Eosinophil-induced end-organ damage
- Exclusion of other causes (e.g., parasitic infection, allergy, malignancy, collagen-vascular disease)
- Almost any organ can be affected, but most patients have bone marrow, cardiac, and central nervous system involvement.
- It is characterized by more than 1500 eosinophils/l-JI of peripheral-blood for 6 months or longer.
- It may also follow lung and bone marrow transplantation.
- Lungs, liver, spleen, skin, nervous system may be affected.
- Multisystem injury and organ damage caused by excessive numbers of eosinophils in the body.
- The disease is one of the myelodysplastic disorders.
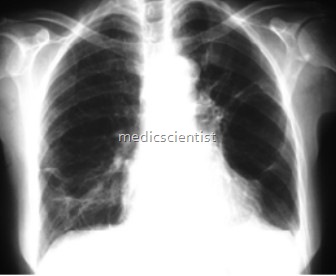
- There is dyspnoea, cough, crepts in lungs, of unknown cause.
- There may be tricuspid valve abnormalities, endomyocardial fibrosis, restrictive cardiomyopathy with tissue infiltration by eosinophils.
Pathophysiology HYPEREOSINOPHILIC SYNDROME
- Organ damage is similar among HES subsets and results from high eosinophil levels.
- Cytokines IL-3, IL-5, and GM-CSF stimulate bone marrow eosinophil production; IL-5 is most specific.
- Blood levels, organ migration regulated by chemokines, especially IL-5 and eotaxins
- HES: Eosinophils infiltrate organs and release toxic granules containing major basic protein, eosinophil peroxidase, eosinophil cationic protein (ECP), eosinophil-derived neurotoxin (EDN), Charcot Leyden crystal, VIP, and substance P. Neurotoxic, cytotoxic, and prothrombotic; creates oxidative burst, reactive oxygen species
- Cytokine release (IL-1, IL-3, IL-5, TNF-) incites damage and activates inflammatory pathways.
- EDN and ECP activate fibroblasts: Fibrosis and organ dysfunction
History —
- Cardiac manifestations (50–60%) may cause heart failure symptoms and chest pain.
- Cutaneous manifestations (50%) may cause pruritus.
- Fatigue, anemia
- GI manifestations (20–30%):
- Gastritis/enteritis: Diarrhea, vomiting, abdominal pain (embolic bowel infarction)
- Hepatic manifestations of hepatitis, Budd-Chiari syndrome
- Left upper quadrant pain (from splenomegaly)
- Neurologic manifestations (50%) may result from thromboembolic disease: Behavioral changes, memory loss, confusion.
- Ocular manifestations (20%): Blurry vision/blindness from microemboli
- Other: Myalgias, arthralgias
- Pulmonary manifestations (40%) may cause nonproductive cough.
Differential Diagnosis HYPEREOSINOPHILIC SYNDROME
- Extensive; first rule out secondary causes of eosinophilia: Parasitic infection, allergy, malignancy, drug hypersensitivity, connective-tissue disorders
- Chronic eosinophilic leukemia: Clonality like F/P+ HES but differs by having 2–20% blasts peripherally or 5–20% blasts in the marrow
- Acute eosinophilic leukemia: A form of AML with 50–80% eosinophils; may cause bronchospasm, heart failure
- Other conditions with high eosinophil levels: Hodgkin lymphoma, mastocytosis, chronic myelomonocytic leukemia (eosinophil variant), cutaneous T-cell lymphoma, Churg-Strauss syndrome/other vasculitides, toxicity (the eosinophilia–myalgia syndrome), HIV, HTLV, bronchopulmonary aspergillosis
Treatment Of HYPEREOSINOPHILIC SYNDROME
First Line
- Treatment with corticosteroids orally or IV
- Dosage and duration are dependent on the patient’s condition.
- Treatment for 2–4 weeks beyond clinical improvement has been suggested.
- Discontinuing offending drug.
- Treatment of underlying parasite infestation
Second Line
- Some patients may require oxygen therapy.
Some Spatial —
- Glucocorticoids Hydroxyurea
- Anticoagulants for patients with thromboembolic complication; corticosteroids.
- Patients unresponsive to corticosteroids have shown marked improvement when given cytotoxic agents such as hydroxyurea
- Treatment of associated conditions.