Article Contents ::
- 1 Pneumothorax Symptoms Causes Diagnosis Treatment with emergency
- 2 what is pneumothorax
- 3 History and Examination
- 4 Risk Factorsfor Pneumothorax
- 5 Spontaneous pneumothorax:
- 6 Classification of pneumothorax
- 7 Traumatic pneumothorax:
- 8 Pathology/Pathophysiology of Pneumothorax
- 9 Spontaneous pneumothorax
- 10 Traumatic pneumothorax
- 11 Tension pneumothorax
- 12 Tension pneumothorax is a medical emergency _
- 13 Primary spontaneous pneumothorax Causes:
- 14 Treatment is simple aspiration.
- 15 Secondary Spontaneous Pneumothorax Causes:
- 16 Treatment
- 17 Traumatic Pneumothorax
- 18 Tension Pneumothorax
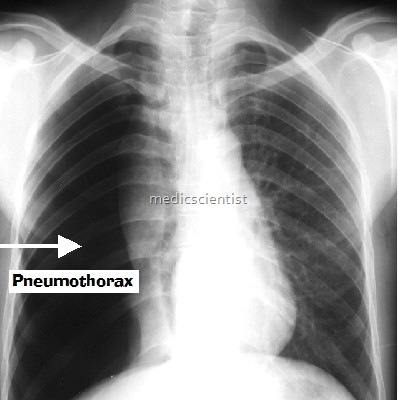
- 19 Diagnosis Pneumothorax
- 20 Treatment of Pneumothorax
- 21 Tension pneumothorax (emergency) :
- 22 Small pneumothorax
- 23 Moderate pneumothorax
- 24 Recurrent pneumothoraces
- 25 Surgery/Other Procedures for pneumothorax
Pneumothorax Symptoms Causes Diagnosis Treatment with emergency
what is pneumothorax
pneumothorax is presence of air in pleural space. The gas enters as the result of a perforation through the chest wall (e.g., due to traumatic or iatrogenic injury) or the pleura (e.g., from the rupture of an emphysematous bleb or superficial lung abscess). Air in the pleural space (the potential space between visceral and parietal pleura). Other variants depend on the substance in the pleural space (e.g. blood: haemothorax; lymph: chylothorax). Accumulation of air or gas between the parietal and visceral pleurae Spontaneous pneumothorax (SP) may be primary (PSP) or secondary (SSP).
History and Examination
- History
- May be asymptomatic if pneumothorax is small.
- Sudden onset breathlessness or chest pain, especially on inspiration.
- Distress with rapid shallow breathing if tension pneumothorax.
- Examination
- Signs may be absent if small.
- Signs of respiratory distress with reduced expansion, hyper-resonance to percussion, breath sounds.
- Tension: Severe respiratory distress, tachycardia, hypotension, cyanosis, distended neck veins, tracheal deviation away from side of pneumothorax
Risk Factorsfor Pneumothorax
Spontaneous pneumothorax:
- Cigarette smoking
- Rupture of superficial lung bulla after coughing or blowing into a musical instrument
- COPD (emphysema), asthma
- Pneumonia: Pneumocystis pneumonia
- Cystic fibrosis
- Neoplasms
- Pneumoconioses
- TB
- Bronchial obstruction
- Flying when pressurization is lost
- Scuba diving
- Catamenial pneumothorax (thoracic endometriosis)
- Connective tissue disorders (Marfan or Ehlers-Danlos syndrome)
- Homocystinuria
Classification of pneumothorax
Traumatic pneumothorax:
- Trauma (penetrating injury, broken rib, ruptured bronchus, perforated esophagus)
- Iatrogenic/post procedures: Intubation, central line placement, liver biopsy, mechanical ventilation, thoracentesis, cardiac pulmonary resuscitation (CPR) (seen in 3% of intensive care unit [ICU] patients)
- Self-inflicted in IV drug abusers (attempting to access internal jugular vein)
Pathology/Pathophysiology of Pneumothorax
- Air is drawn into the negative intrapleural space equalizing pressures and resulting in chest wall expansion, lung collapse, alveolar compression and atelectasis. Mediastinal shift and great vein compression in a tension pneumothorax compromise cardiac function
Spontaneous pneumothorax
- is entry of air in pleural space without any trauma to thorax.
- Primary spontaneous pneumothorax means entry of air in pleural space without any trauma and without any underlying lung disease.
- Secondary spontaneous pneumothorax is entry of air in pleural space with underlying lung disease but without any trauma.
Traumatic pneumothorax
- occurs due,to penetrating or non-pepetrating chest injuries.
Tension pneumothorax
- is a pneumothorax in which pressure in the pleural space due to air is always present throughout the respiratory cycle. There is no negative pressure’.
Tension pneumothorax is a medical emergency _
Primary spontaneous pneumothorax Causes:
- Rupture of apical pleural bleb
- Pres”ence of small cystic spaces under visceral pleura
- Occurs in smokers
- Patients may have sub-clinical underlying lung disease
- There is usually a recurrence.
Treatment is simple aspiration.
- For recurrent pneumothorax thoracoscopy with stapling of blebs, and pleural abrasion.
- pneumothorax catheter is used.
- needle decompression pneumothorax
Secondary Spontaneous Pneumothorax Causes:
- – COPD
- – Other lung diseases.
Treatment
- Tube thoracostomy with injection of sclerosing agents like Doxycline in pleural cavity
- Bleb resection
- Pleural abrasion.
Traumatic Pneumothorax
- Occurs due to penetrating and non-penetrating in-
- jury to chest. ‘
- If there is hemopneumothoraxone tube is placed in superior part of thorax and another in inferior part.
- The upper tube removes air through it and lower tube removes blood from pleural cavity.
- Pneumothorax can also result by needle aspiration, thoracentesis, central IV catheters.
- Treatment is symptomatic ox en thera tlon, tube t oracostomy.
Tension Pneumothorax
- Common causes are mechanical ventilation and cardiorespiratory resuscitation.
- Positive pressure in pleura causes decreased ventilation, decreased venous return, decreased cardiac output.
Diagnosis Pneumothorax
- Enlarged hemithorax, no breath sounds, mediastinal shift to opposite side .
- Tension pneumothorax is a medical emergency as patient can die due to hypoxia and decreased cardiac output.
Treatment of Pneumothorax
- 100% O2 accelerates rate of absorption; if small (<2 cm) and asymptomatic PSP, patient may be observed with no further intervention.
- A large-bore needle should be inserted into second intercostal space anteriorly.
- A thoracostomy tube may be inserted.
Tension pneumothorax (emergency) :
- Maximum O2, insert large-bore needle into second intercostal space, midclavicular line, on side of pneumothorax to relieve pressure, insert chest drain soon after.
- needle decompression pneumothorax may be used,
Small pneumothorax
- (<15–20%): If there is no underlying lung disease, pleural fluid or clinical compromise, give reassurance, analgesia if required and advice on avoiding air travel for at least 6 weeks.
- Intrapleural doxycycline: 5 mg/kg in a total volume of 50 mL
- Intrapleural talc: 5 g in 250 mL isotonic saline; more effective than tetracycline derivatives, but safety concerns exist
Moderate pneumothorax
- (>20%): Aspiration, under local anaesthesia, using a large-bore cannula inserted into the second intercostal space in the midclavicular line, with a three-way tap.
- Up to 2.5 L of air can be aspirated (stop if patient repeatedly coughs or resistance is felt).
- Follow-up CXR should be performed just after, 2 h and 1 week later.
- Chest drain should be inserted if aspiration fails, there is fluid in the pleural cavity or after decompression of a tension pneumothorax. It is inserted into the 4–6th intercostal space in midaxillary line.
Recurrent pneumothoraces
Surgery/Other Procedures for pneumothorax
- Stable PSP (>2 cm): Simple aspiration: Insert 16-F cannula into 2nd anterior intercostal space at midclavicular line and attach a 3-way stopcock and 60-mL syringe.
- pneumothorax catheter ,
- needle decompression pneumothorax
- Manually withdraw air. Close stopcock and repeat CXR after 4 hours.
- Remove if lung reexpanded. Observe patient 2 more hours. Similar outcomes and shorter hospital stay when compared to tube thoracostomy