REGIME FOR MANAGEMENT OF AMI
- Twelve lead ECG is done.
- Or If there is ST elevation more than 1 mm in any lead or 2 mm in V1′ V2 ,
- In comparison, fibrinolytic therapy has largely not been effective in patients with a non-ST elevation MI (NSTEMI)
- then reperfusion therapy is given with streptokinase, tPA, or APSAC by IV infusion or percutaneous coronary intervention. (PCI).
- A potential method of shortening the in-hospital time to fibrinolysis is use of an ECG-based fibrinolytic predictive instrument (TPI)
for more information management-of-acute-myocardial-infarction-ami
Morphine I analgesics
- Aspirin + Clopidogrel – 2 tabs of 300 mg each to be chewed.
- Low molecular weight heparin.
- NTG infusion (nitroglycerine) GP IIb I IIIa antagonist.
- Avoid steroids, NSAIDS, except aspirin.
Thrombolysis in Acute MI
- tPA – tissue plasminogen activator. tPA is more effective than STK.
- Streptokinase – 1.5 million units in 100 ml normal saline IV is given in 60 minutes.
- APSAC-Anisoylated plasminogen strepto-kinase activator complex – !V bolus 30 mg in 5 minutes.
- rPA-retiplase-recombinant tissue plasminogen activator
TIMI Grade —
- Grade 0 — Complete occlusion.
- Grade I — Some penetration of contrast material but no perfusion of distal coronary bed.
- Grade II — Perfusion of entire infarct vessel – with delayed flow.
- Grade III –Full perfusion of vessel with normal flow.
Aim of Thrombolysis is to achieve TIMI III flow
- TIMI frame count – Number of frames for dye to flow from origin of vessel to target.
- TIMI myocardial perfusion grade – Rate of entry and exit of contrast dye from myocardium.
Benefits of thrombolytic therapy
- Decreases mortality
- Decreases infarct size Limits LV dysfunction
- Decreases incidence of malignant ventricular arrh thmias.
Hibernating Myocardium
- Is poorly contracting myocardium due to stenosed , infarct related artery, improves after reperfusion.
GP lIb / IlIa antagonist
- A new regime is to give reduced dose ofthrombolytics plus IV Gp IIb I IIIa antagonist.
Contraindications of STK and other thromboIytics
- Cerebral haemorrhage
- Cerebro vascular accidents in past one year
- Hypertension – systolic blood pressure> 180 mmHg and diastolic blood pressure> 110 mmHg
- Aortic dissection
- Elderly.
Relative Contraindications
- PT – INR more than 2
- Recent surgery
- Recent intervention
- CPR of more than 10 minutes .
- Bleeding diathesis
- Pregnancy
- Haemorrhagic diabetic retinopathy
- Peptic ulcer
- Severe hypertension
- H/o of STK infusion in 5 days to 2 years.
Untoward effects of Streptokinase
- Hypotension
- Allergy
- Haemorrhage_(haemorrhagic stroke in 0.5 to
- 0.9%, specialy in older patients).
Oxygen
- Check SP02 and give 02 inhalation 2 to 4 L/min for 12 hours. – –
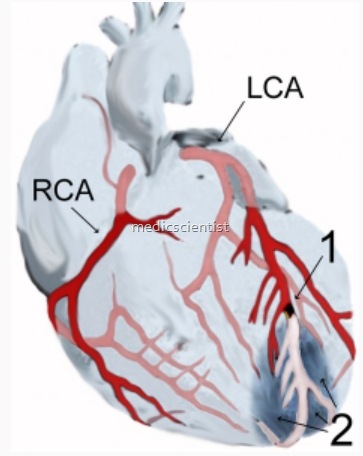
Indications of Coronary Angiography in AMI
- Persistent chest pain
- ST elevation for more than 90 minutes
- Recurrent chest pain
- Recurrent ST elevation.
- Revascularization is done as required by percutaneous coronary intervention (PCI) or coronary artery bypass graft surgery.
Rescue Angioplasty
- If coronary ischemia persists despite thrombolytic therapy then PCI — angioplasty with or without stent is_required.
- Primary percutaneous coronary intervention (PCI) is now preferred for most patients if it can be performed by an experienced operator with less than a 90 minute
Primary PCI
- Angioplasty with or without stenting in first few hours of AMI is primary PCI.
- It should only be done in centers of excellence, experience, and only it can be done as fast as IV, STK.
