Aortic Stenosis PHYSICAL FINDINGS Aortic Stenosis SYMPTOMS, PATHOPHYSIOLOGY with Aortic Stenosis TREATMENT
Aortic Stenosis Definition —
Aortic stenosis is the narrowing of the left venticular outlet usually at the valve. Aortic stenosis is the commonest valvular heart disease in adults and elderly persons. It is more common in males. Aortic Stenosis An impairment of blood flow from the left ventricle to the aorta, as a result of aortic valve disease or obstructions just above or below the valve Aortic Stenosis causes Left ventricular outflow obstruction in adults is most often due to aortic valve stenosis; less common causes are subvalvular or supravalvular disease
Aortic Stenosis ETIOLOGY
- This may result from inflammatory disorders, or excessive development, embryonic maldevelopment, hypertrophy and thickening of a sphincter muscle, of fibrous tissue.
- Rheumatic valve disease
- Aortic sclerosis
- Degenerative / calcific / senile
- Rheumatic heart disease
- Calcific disease of a trileaflet valve
- Congenital AS
- – Bicuspid aortic valve
- – Subaortic stenosis-Discrete
- – Supra valvular AS
- Hypertrophic cardiomyopathy (also called IHSSIdiopathic hypertrophic subaortic stenosis).
Aortic Stenosis PATHOPHYSIOLOGY
- There is obstruction at the outlet of the left ventricle. his leads to increased pressure in the left ventricle and decreased pressure in the aorta.
- Rheumatic valve disease is characterized by fusion of the commissures between the leaflets, with a small central orifice.
- The LV hypertrophies and maintains the cardiac out Jut. As the disease becomes chronic, the LV dilates a d the cardiac output falls.
- hen there is severe obstruction to LV outflow, the Peak systolic pressure gradient (difference of pres: e between LV and aorta) is more than 50 mmHg : d area of aortic orifice is less than 1 cm2•
- Many of the risk factors for atherosclerosis are also associated with aortic valve sclerosis,
- adually LVEDP (left ventricular end diastolic pressure) rises and there is left ventricular failure. The , LA, PA and RV pres;iures increase.
Aortic Stenosis SYMPTOMS OF AORTIC STENOSIS
- Patient may be asymptomatic for many years.
- Patient has exortional dysnoea is due to increased LV diastolic pressure creased pulmonary capillary pressures.
- Angina pectoris is due to LV hypertrophy (increased ement of oxygen), decreased supply due to outflow obstruction and sometimes coincidental coronary artery disease.
- Many patients with mild or moderate aortic stenosis (e.g., with a valve area that is more than 1 cm2 or a valve gradient that is less than 50 mm Hg)
- Syncope is due to vasodilatation of exercising muscles resulting in decreased cardiac output.
- Syncope usually occurs only during exertion.
- Later there is weakness, fatigue, peripheral cyanosis and other features of low cardiac output.
- There is orthopnea, paroxysmal nocturnal dyspnoea, and other symptoms of pulmonary edema and LV failure.
- However, in patients with known AS who are followed prospectively, the most common symptoms are decreased exercise tolerance and dyspnea on exertion.
- Very late findings are pulmonary hypertension with right ventricular failure, systemic venous congestion, hepatomegaly, atrial fibrillation, tricuspid regurgitation.
- When aortic stenosis occurs along with mitral stenosis, there is severe reduction in cardiac output and severe symptoms early in the course of the disease.
- When aortic stenosis occurs along with aortic regurgitation, there is early left ventricular failure and pulmonary edema.
Aortic Stenosis PHYSICAL FINDINGS
- Rhythm is regular. If there is coexistent MS or MR there is atrial fibrillation.
- Blood pressure is usually normal. Later there is fall in systolic pressure and narrow pulse pressure.
- The presence of hypertension rules out severe aortic stenosis.
- A slow rate of rise in the carotid pulse Mid to late peak intensity of the murmur Reduced intensity of the second heart sound
- The murmur of aortic stenosis is best heard by placing the stethoscope over the base of the heart.
- Peripheral arterial pulse is slow and delayed called pulsus parvus et tardus.
- A bisferiens pulseis found in AS with AR or severe AR but never in pure AS.
- Palpation of the arteries in severe aortic stenosis may reveal a delayed and weakened pulse (e.g., at the carotids).
- The sound is typically described as being “diamond-shaped”;i.e., it starts softly, increases in intensity, and then diminishes to a whisper
- In the late stages of AS the pulse is very low volume and so the delay in upstroke is difficult to feel.
- JVP is normal but in greatly hypertrophied interventricular septum the RV cavity is reduced and there may be a prominent ‘a’ wave in the JVP.
- The left ventricular impulse is displaced laterally and downwards due to left ventricular hypertrophy.
- In pure AS, the left ventricular hypertrophy is a concentric hypertrophy and therefore apex may not be shifted grossly.
- In the left lateral position a double apical impulse may be felt as in IHSS.
- A systolic thrill is present at the base of the heart (right second intercostal space and left third intercostal space), in the jugular notch and along the carotid arteries.
- Systolic thrill is always present in AS except in very mild AS.

Aortic Stenosis Auscultation
- There is an early systolic ejection sound (an opening snap of the aortic valve) heard in noncalcific valvular AS as in congenital AS in children.
- Ejection sound is absent in calcified and rigid valves. The A2 is delayed, (normally A2 or aortic closure sound comes before P2 or pulmonary closure sound) and may overlap the P2. If it is further delayed as in severe AS then it may come after P2. This is called paradoxic or reversed split of S2′
- A2 is heard only if aortic valve is noncalcified and mobile.
- S4 is audible at the apex when there is LV hypertrophy and increased LV end diastolic pressure.
- S3 is heard when the LV dilates and there is frank or incipient heart failure.
- The characteristic murmur of AS is ejection systolic or mid-systolic murmur beginning just after S1′
- This increases in intensity and reaches a peak around the middle of ejection. The murmur then diminishes in intensity gradually and ends just before aortic valve closure (AJ.
- It is low pitched, rough and rasping in character, best heard at the base of the heart i.e. right second intercostal space and the left third intercostal space.
- It radiates along the carotid arteries upwards in the neck.
- It increases in expiration.
- In IHSS the murmur increases on standing but in valvular aortic stenosis the murmur decreases on standing.
- The systolic murmur may also be heard at the apex. The murmur is intense and usually loud i.e. grade III and above.
- In severe AS with heart failure, the apex is feeble and the murmur is soft.
INVESTIGATIONS in Aortic Stenosis

Aortic Stenosis ECG :
- ECG shows LVH, ST de ression, T inversion in Ll’ AVL, and left precordial leads.
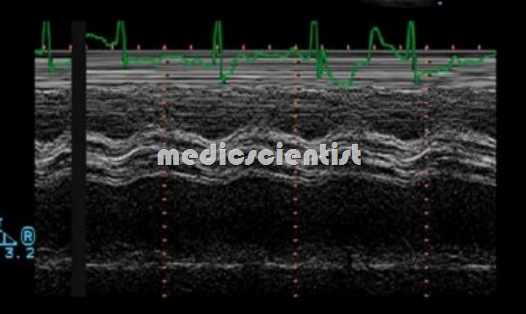
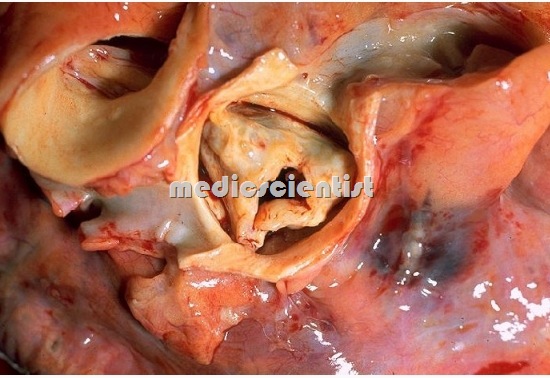
Aortic Stenosis Echocardiography :
- · There is LV hypertrophy
- · Calcification of aortic valves may be seen
- · Congenital bicuspid aortic valve may be diagnosed by eccentric aortic valve cusps.
- · There may be thickened aortic cusps and root
- · TEE shows the obstruction clearly
- · Doppler echocardiography measures LV function and associated AR
- · Other valvular diseases can be seen
- · Supravalvular, valvular and subvalvular AS and IHSS (Idiopathic Hypertrophy Subaortic Stenosis) can be distinguished.
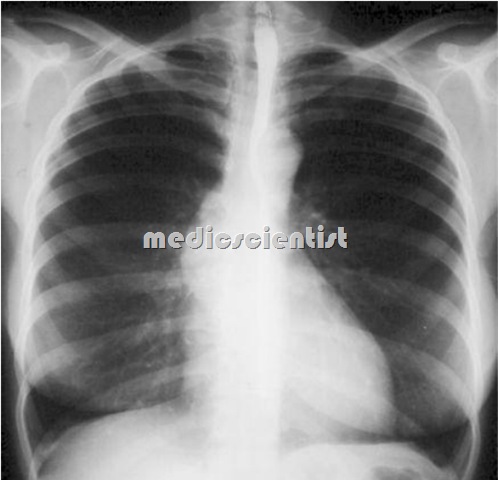
Aortic Stenosis X–ray:
- · LVH
- · Post-stenotic dilatation of ascending aorta in
- severe AS.
- · Aortic calcification in fluoroscopy.
- · Pulmonary congestion
- ·LAE
Aortic Stenosis Catheterization:
- Before operative treatment catheterization of left side of heart and coronary arteriography should be done to :
- · Rule out coronary artery disease
- · Multivalvular disease
- · Feasibility of balloon valvotomy of aortic valve
- · Level of obstruction of the LV outflow
Aortic Stenosis PROGNOSIS
- The average time a patient of AS lives after development of angina pectoris is 3 years, after syncope is 3 years, after dyspnoea is 2 years and after CHF is 2 years.
Aortic Stenosis TREATMENT
- A congenitally bicuspid valve is a common cause of aortic stenosis requiring surgery in all age groups.
- The only definitive therapy for aortic stenosis is aortic valve replacement.
- In severe AS i.e. valve area less than 1 sq cm patient should avoid any physical strain even if asymptomatic.
- Salt restriction, and diuretics for heart failure Digitalis glycosides for heart failure Nitroglycerin for angina pectoris
- Among the 7 percent of patients who underwent surgery at ≤ 50 years of age, approximately two-thirds had a bicuspid valve and one-third had a unicuspid valve.
- Among the remaining patients over age 70, approximately 60 percent had a tricuspid valve and 40 percent had a bicuspid valve.
- Among the 40 percent of patients who underwent surgery between the ages of 50 and 70, approximately two-thirds had a bicuspid valve and one-third a tricuspid valve; a unicuspid valve was rare.
- Statins for prevention of calcification and aortic valve shrinkage in degenerative AS.
- Surgical treatment is AVR (aortic valve replacement). AVR is indicated in severe AS (valve area <1 sqcm), symptomatic patients, patients with LV dysfunction.
- In asymptomatic AS, if ejection fraction is more than 50%, AVR is not done especially in calcific AS, even if severe.
- Surgery should be done before LV failure occurs and ejection fraction falls.
- Operative risk is 4% in most cases but 20% in patients of LVF.
- Aortic valvuloplasty: Percutaneous balloon aortic valvuloplasty can be done in children and young adults with non-calcific AS, and in patients where risk of surgery is high.
PHYSICAL ACTIVITY AND EXERCISE —
- the presence of severity of aortic regurgitation, and the presence of aortic root dilatation.
- Recommendations for physical activity and exercise in patients with bicuspid aortic valves needs to take into account three issues: the presence and severity of aortic stenosis.
