Article Contents ::
Diabetic nephropathy (DN) Renal Long-Term complications of DM (Diabetes Mellitus)
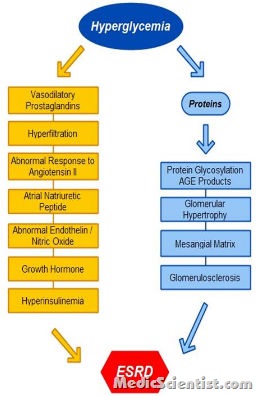
Diabetic nephropathy (DN) is responsible for high morbidity and mortality. DN is associated with diabetic retinopathy and hyperglycemia. DN is due to the effect of growth factors, Angiotensin Il, endothelin, AGEs. A high body mass index (BMI) has been associated with an increased risk of chronic kidney disease among patients with diabetes

- Smoking aggravates renal disease Diabetic nephropathy (DN) Renal complications of DM.
- In Type I and Type Il DM sequence of events is same.
- There is increase in glomerular filtration rate (GFR), there is thickening of glomerular basement membrane, glomerular hypertrophy, and GFR returns to normal.
- After 5 – 10 yrs of type I DM most patients have albuminuria.
- Microalbuminuria is 30 – 300 mgjday in 24-hour urine sample or 30 – 300 IJgjmg creatinine in a spot collection.
- Overt proteinuria is more than 300 mgjday. Blood pressure may be normal.
- With overt proteinuria GFR decreases and after about 7 years end-stage renal disease (ESRD) occurs. Overt nephropathy is irreversible.
- In type Il DM microalbuminuria and even overt nephropathy may be present at the time of diagnosis. In Type Il DM usually there is hypertension with nephropathy. ,
- In type Il DM albuminuria may be due to hypertension, congestive heart failure, prostatic disease, or infection, besides nephropathy.
- Renal tubular acidosis type IV (hypo-reninemic hypoaldosteronism) may occur in type I or II DM.
- There is hyperkalemia, increased with ACE inhibitors (angiotensin converting enzyme inhibitors) and ARBs (Angiotensin receptor blockers).
- There is increased risk of nephrotoxicity with radio contrast especially in patients with nephropathy and volume depletion.
- Before giving radio-contrast dyes, patients should be given IV fluids and serum creatinine monitored.
- Also, acetyl cysteine – 600 mg BD a day before and on the day of study can protect high risk patients with serum creatinine more than 2.4 mg/ dl.
PATHOLOGY Diabetic nephropathy (DN) Renal complications of DM —
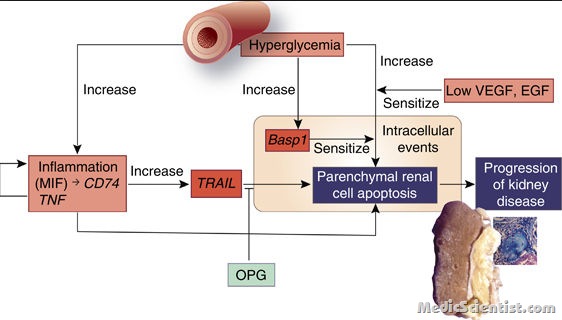
- different pathogenetic processes leading to the pathologic mechanisms in diabetic nephropathy.
- Pathologic abnormalities are noted in patients with long-standing diabetes mellitus before the onset of microalbuminuria.
- There are three major histologic changes in the glomeruli in diabetic nephropathy:
- mesangial expansion; glomerular basement membrane thickening; and glomerular sclerosis
Treatment of Renal complications of DM (Diabetes Mellitus)
- Prevention is by detection of microalbuminuria and treating it by strict blood pressure control, controlling blood sugar, ACE inhibitors, ARBs, lipid lowering drugs.
- Angiotensin converting enzyme inhibitors or angiotensin II receptor blockers have been evaluated for efficacy in the primary prevention of diabetic nephropathy
- When the renal function declines insulin requirement falls because kidney is the site of insulin breakdown.
- Sulphonylureas and Metformin are contraindicated in advanced renal failure.
- BP Strict blood pressure control
- should be maintained at less than 130/80 mm in patients without proteinuria.
- Strict blood pressure control is important for preventing progression of diabetic nephropathy and other complications in patients with type 2 diabetes,
- For patients with microalbuminuria or overt nephropathy BP should be maintained at less than 125 / 75.
- In patients of Type I and II DM with microalbuminuria ARBs and ACE inhibitors must be prescribed.
- ACE inhibitor in type 1 diabetes can be demonstrated early in the course of the disease when microalbuminuria is the only clinical manifestation
- Dose of ACE inhibitors and ARBs should be increased after 3 months to a maximum so as to stop albuminuria.
- If there are side effects with ACE inhibitors like hyperkalemia, cough or, if, ACE inhibitors cannot be given due to renal insufficiency, then calcium channel blockers may be used.
- ACE inhibitors may be recommended in Type I DM and ARBS in type II DM.
- Protein restriction to 0.8 gm/Kg/day may be advised.
- In ESRD hemodialysis may be required.
- In ESRD due to DM there is greater incidence of hypotension, difficult vascular access, retinopathy. Survival is short in patients of ESRD.
- Hyperlipidemia should be treated strictly.
- Renal transplant from a related donor may be done with chronic immunosuppression.
- Combined pancreas and kidney transplant is best but requires great expertise.
