Infective Endocarditis CLINICAL FEATURES of infective Endocarditis (IE) causes the Infective Endocarditis With TREATMENT of infective Endocarditis (IE)
Proliferation of microorganisms on the endothelium of heart results in infective endocarditis. The typical feature–of the· disease is vegetation. Endocarditis may be caused by any microorganism; of streptococci or staphylococci; Haemophilus spp. or other HACEK bacteria Vegetation is a mass of platelets, fibrin, microcolonies of microorganisms and inflammatory cells –

Hacek bacteria is the commonest cause of Infective Endocarditis this group is combined of (e.g., Actinobacillus Eikenella corrodens, or Kingella kingae actinomycetem comitans, Cardiobacterium hominis, ); chlamydiae; enteric bacteria; ricksettsiae; or some time fungi.
Vegetation may form on :
- heart valves
- low pressure side of VSD (ventricular septal defect)
- Mural endocardium (damaged by jet of blood or foreign bodies)
- Intracardiac devices
Infective Endocarditis is the same process occurring in :
- Endocarditis is usually the consequence of two factors: the presence of organisms in the bloodstream and abnormal cardiac endothelium facilitating their adherence and growth.
- Arteries,
- Arteriovenous shunt
- Arterio-arterial shunts ex. PDA (Patent ductus arteriosus)
- Coarctation of aorta
Typical features of Acute Endocarditis
- This usually presents as a severe febrile illness with prominent and changing heart murmurs and petechiae.
- · Fever
- · Damage to cardiac structures by the disease
- · Extracardiac sites involved by hematogenous spread
- · Death in weeks, if untreated
Typical features of Subacute Endocarditis
- This should be suspected when a patient known to have congenital
- valvular heart disease develops a persistent fever,
- Structural cardiac damage present before the disease
- · Extracardiac sites usually not involved
- · Embolic events always occur
- complains of unusual tiredness,
- night sweats or weight loss,
- develops new signs of valve dysfunction or heart failure.
- · Slow course, gradually progressive
- · Structural cardiac damage present before the disease
- · Extracardiac sites usually not involved
- · Embolic events always occur
Organism that mainly causes the Infective Endocarditis —
| Streptococcus viridans | From: | |
StaphylococciHACEK —
|
|
|
| Streptococcus bovis | GIT | |
EnteroccciNosocomial :
|
|
Endocarditis may be non–infective, non-bacterial —
NBTE (Nonbacterial thrombotic endocarditis)
- there is – uninfected platelet fibrin thrombus.
- During transient bacteraemia this gets changed to infected vegetation as in MR, AR AS VSD MVP, Degenerative disease of heart valves and congenital heart diseases. .
Marantic endocarditis are uninfected vegetations in:
- SLE
- Malignancy
- Antiphospholipid syndromes
SIGNS and SYMPTOMS for Infective Endocarditis —

CLINICAL FEATURES of infective endocarditis (IE)
- Fever
- Weight loss
- Malaise
- Myalgia
- Chills
- Sweating (diaphoresis) Anorexia
- Arthralgia
- Back pain
- Heart murmurs – Regurgitant murmurs – MR, AR Arterial emboli can go to kidney, spleen, mesentery, brain, peripheral arteries.
- Splenomegaly
- Subungual haemorrhages – also called splinter hemorrhages under the nails over the nail-bed.
- Javeway’s lesions – nodular hemorrhages on the skin Roth spots – flame-shaped hemorrhages seen on the retina by funduscopy
- Petechiae on the skin
- Clubbing’ may be due to embolisation or immune reaction
- Neurologic features like: Brain abscess, convulsions, hemiplegia, coma, pneumococcal meningitis
- Osler’s nodes are painful pulp of terminal digits of fingers
LABORATORY TESTS of infective endocarditis (IE)
- Anaemia
- Circulating immune complexes Decreased serum complement
- Leucocytosis Microscopic hematuria Increased ESR Rheumatoid factor
DUKE‘S CRITERIA FOR CLINICAL DIAGNOSIS
Major
Evidence of endocardial involvement supporting the diagnosis of IE
- New valvular regurgitation (increase or change in pre-existing murmur does not count as a criterion)
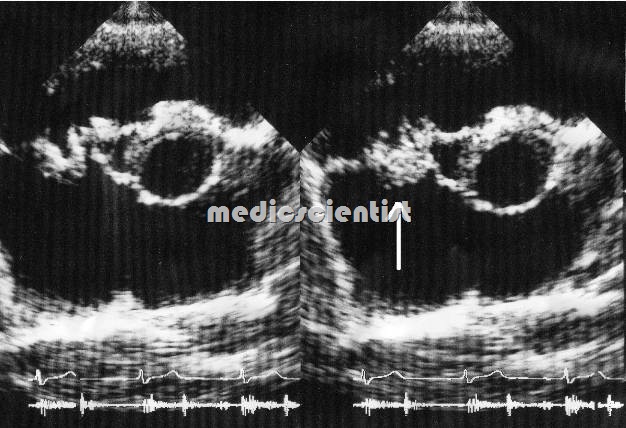
- ·Echocardiography: – Vegetations Abscess
- – Dehiscence of prosthetic valve
- – New valvular regurgitation
- Echocardiogram findings
- (a) Oscillating intracardiac mass present:
- on valve or supporting structures, or
- in the path of regurgitant bloodstream flow, or
- on implanted material, in the absence of an alternative anatomical explanation, or
- (b) Abscess, or
- (c) Newly identified partial dehiscence of prosthetic valve, or
- (a) Oscillating intracardiac mass present:
- Positive blood culture for infective endocarditis
- Persistently positive blood culture, defined as growth and identification of a microorganism consistent with IE originating from:
- blood cultures that are obtained more than 12 hours apart, or
- 3/3 or 3/4 or more separate blood cultures, with the first and last blood cultures obtained at least 60 minutes apart
- Positive blood culture from 2 separate blood cultures or single +ve culture for Coxiella burnetti
- · Evidence of endocarditis
- Expected microorganisms for infective endocarditis from two separate blood cultures – viridans streptococci,* HACEK†groups, Streptococcus bovis, or community-acquired Staphylococcus aureus or enterococci, without known primary focus, or
- Persistently positive blood culture, defined as growth and identification of a microorganism consistent with IE originating from:
Minor
1. Predisposing conditions present like valvular heart disease and h/o recent dental extraction 2. Fever> 100AF 3. Vascular phenomenon:
- Echocardiogram: findings may be consistent with IE, but major criteria as stated above are not met
- Major arterial emboli
- Septic pulmonary infarcts
- Mycotic aneurysms
- Intracranial haemorrhages
- Conjunctival haemorrhages
- Janeway’s lesions
4.Immunologic phenomenon:
- Immunological phenomena present: Roth spots, Osler’s nodes, glomerulonephritis, rheumatoid factor via laboratory analysis
- Glomerulonephritis
- Osler’s nodes
- Roth’s spots
- Rheumatoid factor
5. Microbiology:
- Vascular phenomena present: major arterial emboli, mycotic aneurysm, septic pulmonary infarcts, conjunctival haemorrhages, intracranial haemorrhage, Janeway lesions
- – Positive blood culture
- – Serology positive
- Microbiological evidence of IE: blood cultures are positive but major criteria are not met as previously described,‡ or serological studies support an infection that is consistent with the diagnosis of IE
Application of Duke’s criteria
- 2 Major OR 5 minor OR 1 major and 3 minor criteria Should be present.
- Diagnosis is rejected if symptoms subside in 4 days of antibiotic treatment otherwise alternative diagnosis made.
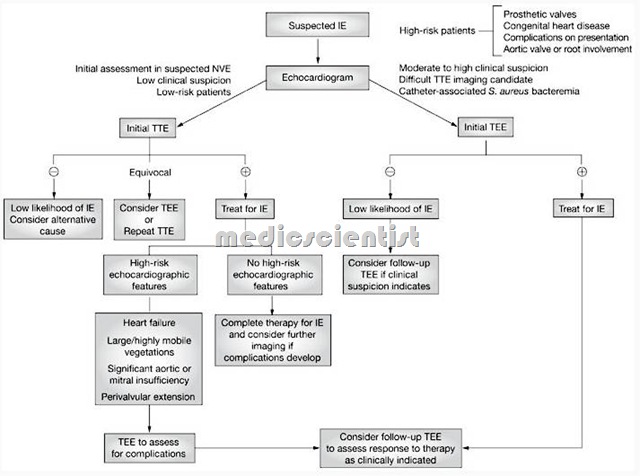
- Standard antimicrobial therapy for infective endocarditis is generally administered to patients characterized as definite or probable by the Duke criteria.
- The diagnosis of infective endocarditis (IE) is usually based upon a constellation of history, clinical findings, laboratory studies etc.
- Treatment is appropriate antibiotic
Streptococcus bovis
- 1. Penicillin G – 2-3 million units 4 hrly for 4 wks.
- + Gentamycin 1 mg/kg 1M I IV 8 hrly for 2 wks .. OR
- 2. Ceftriaxone 2gm/d IV OD for 4 wks.
- OR
- 3. Vancomycin 15 mg/kg/IV 12-hourly for 4 wks.
Resistant Streptococci / Enterococci
- Penicillin G 3-4 million units (MU) 4-hourly
- + Gentamycin 1 mgjkg 1M j IV 8-hrly for 6 wks. OR
- 2. Ampicillin 2 9 IV 4 hly
- + Gentamycin 1 mgjkg IV 8-hrly for 4-6 wks. OR
- Vancomycin 15 mgjkg IV 12-hrly for 4-6 wks + Gentamycin 1 mgjkg IV 8-hrly for 4-6 wks.
Staphylococi
- Methicillin-susceptible strains
- 1. Nafcillin 2g IV 4 hly for 4-6 weeks
- + Gentamycin 1 mgjkg 1M j IV 8 hly for 3-5 days
- OR
- 2. Vancomycin 15 mgjkg 1M j IV 8 hrly for 4-6 wks
- Methicillin-resistant strains
- 1. Vancomycin, 15 mgjkg 1M j IV 8 hrly for 4-6 weeks
For Prosthetic Valve Endocarditis
- Nafcillin + Gentamycin + Rifampicin (300 mg OD 8 hrly) for 6 wks.
For Methicillin-resistant Prosthetic Valve endocarditis
- Vancomycin + Genticin + Rifampicin
HACEK (Hemophilus, Actinobacilus, Cardiobacterium, Eikenella, Kingella)
- Ceftriaxone 2 gm IV OD for 4 weeks.
