Article Contents ::
Inflammatory Bowel Diseases
Inflammatory Bowel Disease (I BD) is an idiopathic and chronic intestinal inflammation.
- It is of 2 major types :
- Ulcerative colitis UC)
- Crohn’s diseas (C.D)
- The factors associated with increased incidence of IBD are smoking, oral contraceptive, family history, genetic predisposition, hypogammaglobulinaemia, emotional stress.
- The term for a number of chronic, relapsing inflammatory diseases of the gastrointestinal tract of unknown etiology.
- The two most common types are ulcerative colitis and Crohn’s disease.
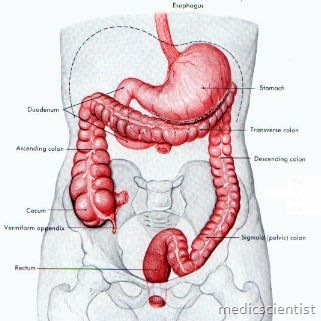
- UC affects the colon, whereas CD can involve any component of the gastrointestinal tract from the oral cavity to the anus.
- Age of onset is 15-30 years and 60-80 years.
- It is equally common in males and females.
Clinical features of Crohn’s disease
- There is pain in right lower quadrant of abdomen, diarrhea, palpable mass sometimes, fever, anorexia, fear of eating.
- Afl inflammatory mass is palpable in right lower quadrant sometimes.
- There is bowel obstruction due to progressive narrowing and stricture.
- There may be pain after meals. ~Fistulas are common due to perforation.
DIAGNOSTIC APPROACH —
- The diagnosis of IBD involves five steps.
- The first two are typically performed by the general pediatrician, and the last three are performed by the pediatric gastroenterologist.
- Clinical suspicion of the illness based upon history,
- examination and screening laboratory data Exclusion of other illnesses that have a similar presentation
- Establishment of the diagnosis of IBD, with differentiation between CD and UC
- Localization of the region of the disease Identification of extraintestinal manifestations
Pathology in Ulcerative colitis
- Involves the rectum and extends upwards.
- The mucosa is ede’r1atous, haemorrhagic and ulcerated.
- Pseudopolyps may be present.
- The colon becomes narrowed and shortened.
- There may be perforations. There may be crypt abscesses.
- There may be pseudopolyps or carcinoma in colon. Stricture and obstruction may occur, seen on endoscopy.
In X-ray with barium there is string sisn of narrowed lumen of intestine.
Summary of findings in Ulcerative colitis
- Gross blood in stools
- The onset of symptoms may be insidious, with non-bloody diarrhea and sometimes poor weight gain.
- Mucus in stools
- ANCA (Antineutrophil cytoplasmic antibody) positive Rectum is usually involved
- Patients with UC have colitis affecting the rectum and extending proximally to a variable degree
- The lesions are continuous Strictures are rarely found.
Summary of findings in Crohn‘s disease
- Systemic symptoms are common
- Any part of GI tract, usually terminal ileum and/or colon; transmural inflammation, bowel wall thickening, linear ulcerations,
- Blood and mucus usually not present in stools Abdominal pain is common
- Abdominal mass usually palpable
- There is significant perianal and perineal disease Fistulas are common
- Strictures are frequent
- Intestinal obstruction is common Colonic obstruction is common Responds to antibiotics
- May recur after surgery
- AS CA (Anti Saccharomyces cerevisiae antibody) Rectum is spared
- Fever, abdominal pain, diarrhea (often without blood), fatigue, weight loss, growth retardation in children;
- There is cobblestoning in endoscopy (cobblestones are large cricket ball size stones used for paving paths)
- There may be granuloma on biopsy
- Small bowel may be involved
- There is segmental colitis.
Treatment of Ulcerative colitis
- Treatment for inflammatory bowel disease is Sulphasalazine (4-8 g/day) and other 5-ASA agents dose 2-4 gjday).
- 5 ASA agents are Sulfasalazine, Olsalazine, Asacol, Pentasa.
- For distal disease 5-ASA oral and enema is given. IV glucocorticoids, glucocorticoid enemas.
- IV CSA (cyclosporin), Azathioprine, 6 Mercaptopurine.
Treatment of Crohn’s disease
- 5 -ASA oral or enema Metronidazole
- Ciprofloxacin
- Oral or IV glucocorticoids Azathioprine
- Infliximab
- Total parenteral nutrition (TPN).
Newer therapies
- Anti TNF antibody
- Newer immunosuppressive agents like tacrolimus Surgical therapy for haemorrhage, obstruction, fistula, stricture.
