Article Contents ::
Chronic Long-Term Ophthalmologic Complications of DM (Diabetes Mellitus)
Blindness – occurs due to progressive diabetic Retinopathy and macular oedema. Diabetic retinopathy may be non-proliferative and proliferative. Diabetic retinopathy (DR) is one of the most important causes of visual loss worldwide, and is the principal cause of impaired vision in patients between 25 and 74 years of age. Strict glycemic control early in the course of diabetes and photocoagulation for established disease are of primary importance. Vitrectomy can also be used to preserve useful vision in advanced Chronic Long-Term Ophthalmologic Complications of DM (Diabetes Mellitus) cases and certain circumstances.
Ophthalmologic examination schedule For Prevention ::
| Patient group | Recommended first examination | Minimum routine follow-up* |
| Type 1 diabetes | Within 5 years after diagnosis of diabetes once patient is age 10 years or older | Yearly |
| Type 2 diabetes | At time of diagnosis of diabetes | Yearly |
| Pregnancy in preexisting diabetes | Prior to conception and during first trimester. Counsel on the risk of development and/or progression of retinopathy. | Close follow-up throughout pregnancy and for one year postpartum. |
- Cataract is a major cause of vision impairment in people with diabetes. Numerous studies have documented an association between diabetes and cataracts.
Glaucoma
- Glaucoma is a progressive optic neuropathy associated with typical optic disc changes and visual field defects
Ocular movement disorders
- Extraocular motility disorders may occur in patients with diabetes, secondary to diabetic neuropathy, involving the third, fourth, or sixth cranial nerve
Diabetic papillopathy
- Diabetic papillopathy is an uncommon optic nerve condition characterized by acute disc edema and mild vision loss
Anterior ischemic optic neuropathy
- Anterior ischemic optic neuropathy (AION) is an acute vascular condition of the optic nerve
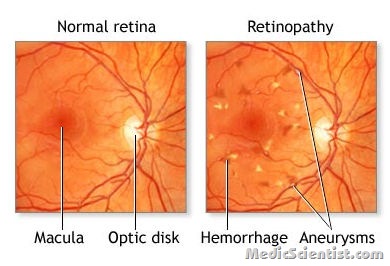
Non-proliferative diabetic retinopathy
- appears in 10-20 years after diabetes.
- There are micro-aneurysms, blot haemorrhages and cotton wool spots,
- intraretinal microvascular damage
- and haemorrhages leading to retinal ischemia.
In proliferative retinopathy
- new vessels appear in macula
- and near optic nerve causing vitreous haemorrhage,
- fibrosis,
- and retinal detachment.
Non-proliferative retinopathy progresses to proliferative retinopathy. Fluorescein angiography is done to detect macular edema. Macular edema is not usually associated with blindness.
Treatment for Ophthalmologic Complications of DM (Diabetes Mellitus)
- Prevention – Blood sugar and blood pressure control delays complications.
- For Diabetic Retinopathy – Prophylactic photo coagulation with intensive therapy.
- Pan retinal laser photocoagulation for proliferative retinopathy.
- Focal laser photocoagulation for macular oedema.
- Aspirin 650 mg/day may be useful.

