Article Contents ::
- 1 Shock
- 2 Aims of Treatment in Shock
- 3 History in Shock
- 4 Risk Factorsfor Shock
- 5 Pathogenesis of Shock
- 6 Systemic vascular response increases so that there is :
- 7 Vasodilator substances in shock:
- 8 Cardiovascular response
- 9 Pulmonary response
- 10 Renal response
- 11 Metabolic effects
- 12 Monitoring the Patient with shock
- 13 TYPES OF SHOCK
- 14 HYPOVOLEMIC SHOCK
- 15 Presentation
- 16 Management
- 17 TRAUMATIC SHOCK
- 18 Management
- 19 INTRINSIC CARDIOGENIC SHOCK
- 20 Treatment —
- 21 COMPRESSIVE CARDIOGENIC SHOCK
- 22 NEUROGENIC SHOCK
- 23 HYPOADRENAL SHOCK
- 24 OTHER THERAPIES IN SHOCK
- 25 SEPTIC SHOCK
Shock
Shock is a clinical syndrome due to inadequate tissue perfusion. A clinical syndrome marked by inadequate perfusion and oxygenation of cells, tissues, and organs, usually as a result of marginal or markedly lowered blood pressure. Shock is the physiologic state characterized by significant reduction of systemic tissue perfusion, resulting in decreased tissue oxygen delivery.
- This leads to Cellular dysfunction leading to production and release of inflammatory mediators which act on the microvasculature.
- Cellular injury —–> Multiple Organ Failure ——> Death
- The cellular injury is reversible or irreversible.
Aims of Treatment in Shock
- Restore perfusion by expansion of blood volume
- Check the cause like:
- – Haemorrhage
- Impairment of cardiac functions
- Infections.
History in Shock
- Hypovolemic shock: Burns, trauma, bleeding wound(s), hematemesis, vomiting, abdominal pain, melena, diarrhea, vaginal bleeding
- Cardiogenic shock: Dizziness, chest pain, dyspnea, palpitations
- Septic shock: Fever, chills, rigors, malaise, myalgias, cough, shortness of breath, productive sputum, dysuria, suprapubic pain, flank pain
- Neurogenic: Spinal trauma
Risk Factorsfor Shock
- Hypovolemic shock: Hemorrhage, dehydration, burns, anaphylactic (decreased effective circulating volume)
- Cardiogenic shock: Heart disease such as MI and congestive heart failure (CHF)
- Septic shock: Elderly, immunosuppression, critical illness, malnutrition, cancer
- Neurogenic: Spinal cord injury
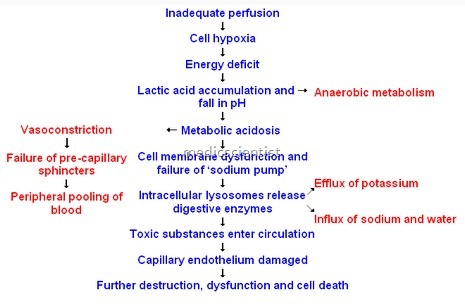
Pathogenesis of Shock
- Cardiac output falls below 60%.
- There is hypotension i.e. mean <60 mmHg.
-
Systemic vascular response increases so that there is :
- Increased perfusion of brain and heart.
- · Decreased perfusion of skin, muscles, GIT. Cerebral and coronary perfusion is maintained spite fall of blood pressure.
- Arterioles have vascular smooth muscle.
- Vascular smooth muscles have Alfa and Beta adrenergic receptors.
- Alfa-1 receptors cause Vasoconstriction.
- Beta-2 receptors cause Vasodilatation.
- Norepinephrine released from efferent sympathetic fibers act on ~ receptors.
- Epinephrine and norepinephrine are released by adrenal medulla.
- Other vasoconstrictors are :
- angiotensin II,
- vasopressin,
- endothelins,
- thromboxane A2.
Vasodilator substances in shock:
- Prostacyclin
- PG 12
- Nitric oxide
- Adenosine.
Derangement of cellular metabolism leads to cell death resulting in organ failure.‘ There is :
- · Hypovolemia
- · Hypotension
- · Hypoxia.
- Autonomic response —> decreased vagal response, increased heart rate, increased cardiac output, increased glycogenolysis and gluconeogenesis.
- Severe pain, severe stress leads to increased ACTH and increased blood volume.
- Release of renin —> Angiotensin I —> angiotensin Il —> Vasoconstriction —> aldosterone release by adrenal cortex —> Vasopressin by posterior pituitary.
- Aldosterone and Vasopressin enhance water reabsorption and cause vasoconstriction.
Cardiovascular response
- Decreased cardiac output
- Decreased stroke volume
- Increased heart rate
- Increased systemic vascular resistance
- Vasoconstriction and peripheral vasoconstriction are compensatory responses.
Pulmonary response
- Tachypnea —> Hypoxia —> Respiratory alkalosis —> Atelectasis —> Acute Lung Injury —> Acute respiratory distress syndrome
Renal response
- Shock —> acute tubular necrosis —> decreased GFR —> increased Angiotensin —> increased aldosterone and vasopressin —> decreased urine formation Low dose dopamine may be useful.
Metabolic effects
- Disruption of Lipid,
- Carbohydrate and protein metabolism.
Monitoring the Patient with shock
- · ICU admission
- · Monitor arterial pressure (intraarterial)
- · Pulse
- · Respiratory rate
- · Urine flow (Foley’s catheter)
- · Mental status
- · Pulmonary arterial catheter (for Right atrial, Pulmonary arterial, and Pulmonary wedge pressure)
- · Cardiac output
- · 02 consumption, 02 delivery
- · Systemic vascular resistance to be maintained.
TYPES OF SHOCK
HYPOVOLEMIC SHOCK
Causes
- · Haemorrhage
- · Loss from GIT, urinary, insensible loss (extravascular fluid sequestration)
- · Tachycardia
Presentation
- Postural hypotension, Severe hypotension
- Oliguria
- Agitation
- Confusion
- Mental obtundation
- Differentiation from cardiogenic shock by absence of S3, rales, jugular venous distension.~
Management
- Give volume:
- · Isotonic saline (2-3 litres in 112 hour)
- · Blood transfusion (0 +ve packed RBCs).
- · Dopamine
- · Vasopressin
- · Dobutamine (No norepinephrine)
- · Oxygen
- · Endotracheal intubation.
TRAUMATIC SHOCK
- · Haemorrhage
- · Hypovolemia
- · Pain
- · Tissue ischemia
- Pericardial tamponade
- Tension Pneumothorax
- Myocardial injury.
Management
- · Airway
- · Breathing
- · Circulation
- · Control haemorrhage
- · Antioxidants.
INTRINSIC CARDIOGENIC SHOCK
- It is complication of Myocardial Infarction.
Presentation
- · Decreased cardiac output
- · Pulmonary congestion
- · Increased systemic vascular resistance / Left ventricular failure / Right ventricular failure / Pulmonary arterial hypertension ~ alveolar edema
- · There is no hypovolemia.
Treatment —
- Management of AMI to be done Dopamine
- Norepinephrine
- Vasopressin
- Dobutamine
- Furosemide
- Intra Aortic Balloon Pump
- Revascularization
- Ventricular Assist Device
- Heart transplantation.
COMPRESSIVE CARDIOGENIC SHOCK
Causes
- · Tamponade
- · Increased intrathoracic pressure
- · Tension pneumothorax
- · Intermittent positive pressure ventilation (excessive)
- ·Acute right heart failure in pulmonary embolism. There is pulsus paradoxus.
NEUROGENIC SHOCK
- · High cervical cord injury
- · Spinal anaesthesia (Cephalad migration)
- · Head injury.
Management
- · Give fluids
- · Norepinephrine.
HYPOADRENAL SHOCK
- Adrenal insufficiency in stress, surgery, illness, trauma, sepsis, (due to previous high dose of exogenous corticosteroids) in patients of :
- · Tuberculosis
- · Metastatic disease
- · Bilateral haemorrhage
- · Amyloidosis
Treatment
- Dexamethasone – 4 mg· IV
- Hydrocortisone – 100 mg IV 6 – 8 hourly.
OTHER THERAPIES IN SHOCK
- · Elevation of foot
- · Pneumatic antishock garment
- · Rewarming.
SEPTIC SHOCK
Systemic responses to infection:
- · Fever
- · Hypothermia
- · Tachypnea
- · Tachycardia.