Article Contents ::
- 1 Urinary Tract Infection (UTI) and Pyelonephritis
- 2 Acute urethral syndrome
- 3 Urinary Tract Infection Etiology
- 4 Urinary Tract Infection Risk Factors
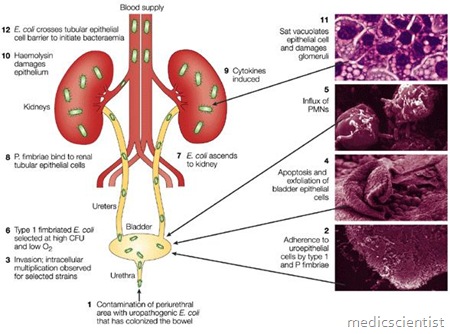
- 5 Route of Infection
- 6 Clinical Presentations Cystitis:
- 7 Acute pyelonephritis :
- 8 Urethritis :
- 9 Catheter-associated UTI
- 10 TREATMENT of Urinary Tract Infection
- 11 Rx for 7-14d for Urinary Tract Infection
Urinary Tract Infection (UTI) and Pyelonephritis
- Urinary Tract infections may be :
- 1. Lower tract infection – Urethritis and cystitis
- 2. Upper tract infection – Acute pyelonephritis, prostatitis, intrarenal and perinephric abscesses.
- Acute pyelonephritis is a syndrome caused by an infection of the renal parenchyma and renal pelvis, often producing localized flank or back pain combined with systemic symptoms such as fever, chills, and nausea. It has a wide spectrum of presentation from mild illness to septic shock.
- Infection of the kidneys, ureters, or bladder by microorganisms that either ascend from the urethra (95% of cases) or that spread to the kidney from the bloodstream (5%).
UTI (Urinary Tract Infection) exists when microorganisms are detected in urine, urethra, bladder, kidney and prostate.
- Growth of >105 organisms/ml from mid-stream clean catch urine samples is diagnostic of infection of urinary tract (UT).
- In symptomatic patients, small number of bacteria may also be diagnosed as UTI.
- Acute symptomatic infections are common in young girls and womer.].
- Urine specimens’may also be collected by suprapubic aspirations and from indwelling catheters in patients.
Acute urethral syndrome
- is dysuria, urgency and frequency without significant bacteriuria.
- UTI (Urinary Tract Infection) may be :
- 1. Catheter-associated or nosocomial.
- 2. Non-catheter-associated or community-acquireLt
Urinary Tract Infection Etiology
- Gram-negative bacteria – Escherichia coli, Proteus, Klebsiella, Enterobacter, Pseudomonas
- Gram-positive bacteria – Staphylococcus aureus Others–Chlamydia trachomatis, Neisseria gonorrhoeae and herpes simplex virus is found in sexually active young women.
- Indwelling catheters
- Renal calculi
- Benign prostatic hyperplasia
Urinary Tract Infection Risk Factors
- Underlying urinary tract abnormalities
- Indwelling catheter
- Recent urinary tract instrumentation
- Nephrolithiasis
- Immunocompromise, including diabetes
- Elderly, institutionalized women
- Prostatic enlargement
- Childhood UTI
- Acute pyelonephritis within the prior year
- Frequency of recent sexual intercourse
- Spermicide use
- Stress incontinence
- Pregnancy
- Hospital-acquired infection
- Symptoms >7 days at presentation
Route of Infection
- Infection enters via the urethra up to the kidneys. The vagina also is a source of infection in females. Hematogenous infection occurs in debilitated and immunocompromised patients.
- Staphylococcus and Candida infections of kidney may follow bacteremia or fungimia from bones, skin and vasculature.
Clinical Presentations Cystitis:
- Symptoms are dysuria, frequency, urgency and suprapubic pain.
- Urine is cloudy with bad odour. There may be hematuria.
- Microscopic examination shows white cells and bacteria.
- There is tenderness in suprapubic area.
- There may be urethritis, vaginitis, and cervicitis In females.
- The presenting symptoms of UTI vary enormously.
- Young patients with bladder infections may have pain with urination;
- urinary frequency or urgency, or both; pelvic or suprapubic discomfort;
- low-grade fevers; or a change in the appearance or odor of their urine.
- Older patients may present with fever, confusion, or coma caused by urosepsis.
Acute pyelonephritis :
- Symptoms develop in a few hours or days.
- There is fever, chills, rigors, nausea, vomiting, diarrhea.
- There is tachycardia, muscle tenderness, abdominal tenderness.
- There may be gram-negative sepsis.
- There is leukocytosis, and bacteria in urine. There may be leukocyte casts, hematuria.
- The symptoms respond to treatment in 2-3 days.
- If there is abscess, urinary obstruction or other local disease, the pyelonephritis becomes chronic and does not respond to treatment.
Chronic pyelonephritis :
- Chronic pyelonephritis is chronic interstitial nephritis due to bacterial infection of the kidney.
Urethritis :
- In women with no bacterial growth in urine culture, the following organisms may be responsible for urethritis – C. trachomatis, N. gonorrhoeae, Herpes simplex virus.
- There is gradual onset of symptorros of UTI, no hematuria, no pain.
- . But there is gross hematuria, suprapubic pain, fever and burning during micturition in E.coli infection.
Catheter-associated UTI
- In 10% of hospitalized patients there is bacteriuria. The causative agents are E.coli, Proteus, Pseudomonas, Klebsiella, Staphylococci, Enterococci and Candida.
- There is higher incidence in prolonged catheterization, severe illness, bad catheter care, and if no antibiotics are given.
- Infection reaches the l;>ladder through the urine in the catheter or from the outside-wall of the catheter.
- Catheter-associated UTI can be prevented by using aseptic technique during insertion, care of catheter to minimize cross infection, antibiotic therapy, closed catheter drainage units, regular change of catheters at few weeks intervals.
TREATMENT of Urinary Tract Infection
- A culture and antimicrobial sensitivity-testing must be done before start of treatment.
- Urinary tract obstruction should be corrected. For lower urinary tract infection, short courses of therapy are given.
- Long-term therapy is given for upper tract infections.
- Recurrence after 2 weeks of therapy may be due to infection with the same strain of bacteria.
- For acute cystitis in females – 3 days or 7 days treatment with amoxycillin, TrimethoprimSulphamethoxazole, Cefpodoxime, Ciprofloxacin, Ofloxacin, Levofloxacin may be given.
- For uncomplicated pyelonephritis in women: Oral or IV QUinolones, Ceftriaxone, Gentamycin IV followed by oral QUinolones for 2 weeks.
- For complicated UTI: Oral quinolones for 2 weeks or IV ampicillin + gentamicin, quinolones, ceftriaxone, or imipenem- cilastatin for 2-3 weeks.