Article Contents ::
- 1 Chronic Hepatitis Classification viral hepatitis Clinical features and Treatment
- 2 Chronic Hepatitis
- 3 Chronic hepatitis may be of three types:
- 4 Other presentations of chronic hepatitis may be
- 5 Classification of Chronic Hepatitis Classification by extent of liver injury
- 6 Classification of Chronic hepatitis by Cause
- 7 Classification of Chronic hepatitis by Grade
- 8 Chronic viral hepatitis generally follows:
- 9 Chronic Hepatitis B
- 10 Hepatitis B virus replication (HBV)
- 11 Clinical features of Chronic hepatitis B
- 12 Laboratory features
- 13 Chronic hepatitis B Treatment
- 14 Chronic Hepatitis D
- 15 Chronic Hepatitis D Treatment
- 16 . Chronic hepatitis C
- 17 Clinical features
- 18 Laboratory features
- 19 Chronic hepatitis C Treatment
- 20 Chronic Autoimmune Hepatitis
- 21 Laboratory features
- 22 Autoimmune Hepatitis Treatment
Chronic Hepatitis
- Chronic hepatitis is a liver disorder with inflammation and necrosis persisting for more than 6 months.
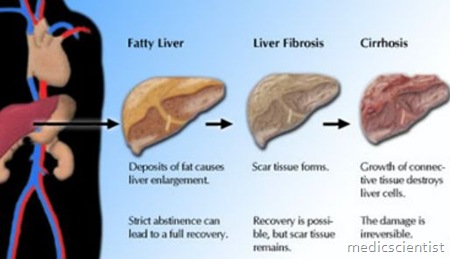
- Chronic hepatitis may be mild, non-progressive, or severe, or may lead to cirrhosis.
Chronic hepatitis may be of three types:
- · Chronic viral hepatitis
- · Chronic drug-induced hepatitis
- · Autoimmune chronic hepatitis.
Other presentations of chronic hepatitis may be
- · Wilson’s disease
- · Alcoho’lic hepatitis.
Classification of Chronic Hepatitis Classification by extent of liver injury
- 1. Chronic persistent hepatitis
- 2. Chronic lobular hepatitis
- 3. Chronic active hepatitis.
Classification of Chronic hepatitis by Cause
- · Hepatitis B
- · Hepatitis B plus D
- · Hepatitis C
- · Autoimmune hepatitis type I, II and III based on serology
- · Drug-associated chronic hepatitis
- · Cryptogenic chronic hepatitis.
Classification of Chronic hepatitis by Grade
- 1. Periportal necrosis
- a. Piecemeal necrosis or interface hepatitis
- b. Bridging necrosis
- 2. Intralobular necrosis
- 3. Portal inflammation
- 4. Fibrosis.
- Viral hepatitis B
- Viral hepatitis C
- Viral hepatitis Band C with superimposed hepatitis D.
- Hepatitis A and E are self-limited and do not progress to chronic hepatitis.
Chronic Hepatitis B
- Hepatitis B infection at birth may be silent but there
- is a 90% chance of chronic infection. •
- In young adults there is overt symptomatic acute hepatitis but progression to chronic hepatitis is rare.
- Chronic hepatitis may be asymptomatic, mild or severe.
- Chronic hepatitis B may progress to severe form, cirrhosis, and liver failure in about a quarter of the cases.
Hepatitis B virus replication (HBV)
- Replicative phase is identified by the presence of serum markers – HBeAg (Hepatitis B e antigen) and HBV DNA, presence of intrahepatocyte antigens HBcAg (Hepatitis B core antigen) and liver injury.
- Non-replicative phase is characterized by absence of HBeAg and HBV DNA, and minimal liver injury.
- Chronic HBV infection at birth and in early childhood leads to hepatocellular carcinoma in a majority of, cases.
Clinical features of Chronic hepatitis B
- · Asymptomatic infection
- · Deblitating disease
- · Progresses to end-stage hepatic failure
- · Onset may be insidious (slow), or chronic disease may follow acute hepatitis B.
- · Fatigue
- · Persistent or intermittent jaundice
- · Malaise, anorexia, leading to slow hepatic decompensation
- · Cirrhosis of liver – ascites, edema, bleeding gastroesophageal varices, hepatic encephalopathy, coagulopathy and hypersplenism.
- Extrahepatic manifestations – arthralgias, arthritis, purpuric lesions due to vasculitis, polyarteritis nodosa.
Laboratory features
- · Amino transferase elevation may be from 100 to 1000 units.
- · ALT (Alanine amino transferase) is elevated more
- than AST (aspartate amino transferase).
- · In cirrhosis AST may be more than A LT.
- · Alkaline phosphatase may be normal.
- · Serum bilirubin may be moderately raised – 3 to 10 mg/dL.
- · Hypoalbuminemia may be present.
- · Prothrombin time increased.
Chronic hepatitis B Treatment
- Progression of disease occurs in patients with active HBV replication.
- Patients with high level HBV replication are at risk of hepatocellular carcinoma.
- Antiviral therapy should be given to all patients of chronic hepatitis B. The drugs for chronic hepatitis B are injectable interferon alpha IFNa, oral lamivudine, oral adefovir dipivoxil.
- Antiviral therapy should be given to patients with detectable· markers of HBV replication, in patients with incr~ased ALT twice the upper limit of normal, all immunocompromised individuals, patients of compensated or uncompensated disease. “,
- Dose of interferon – IFN 5 million units subcutaneous daily for 16 weeks or 10 million units 3 times a week.
- Dose of Lamivudine – Daily oral dose of 100 mg for 12 months.
- Dose of Adefovir – Oral daily dose of 10 mg for 48 weeks (1 year).
Chronic Hepatitis D
- Chronic hepatitis D may follow acute infection with hepatitis B virus.
- HDV infection can increase the severity of acute hepatitis B but progression to chronic hepatitis mayor may not occur.
- If HDV infection occurs in chronic hepatitis B then there is deterioration of liver function resulting in severe liver disease.
- The clinical features of hepatitis D over hepatitis B are same as for chronic hepatitis B alone.
- In chronic hepatitis D, anti-LKM i.e. antibodies to liverkidney microsomes is an important serological feature. This anti-LKM is called anti LKM3 (anti LKM1 is seen in patients with chronic hepatitis C and autoimmune hepatitis).
Chronic Hepatitis D Treatment
- IFN-ex in high doses – 9 million units 3 times a week for 12 months.
- Liver transplantation.
. Chronic hepatitis C
- Acute hepatitis C virus infection may lead to chronic hepatitis C in more than half the cases.
- In chronic transfusion-associated hepatitis there is progression to cirrhosis in l/Sth of cases.
- Even in asymptomatic patients who go for blood donation, hepatitis C may be detected.
- The source of HCV infection may be percutaneous exposure in the past.
- ALT may be normal.
- In patients with normal ALT the disease may not be serious and may not progress to failure and cirrhosis.
- In chronic hepatitis C, progression to liver failure is common with old age, longer duration of infection, histological changes, alcoholic liver disease, chronic hepatitis B, HIV infection, a antitrypsin deficiency.
- Chronic hepatitis C may also convert to hepatocellular carcinoma.
Clinical features
- · Fatigue
- · Jaundice – rarely
- · Sjogren’s syndrome
- · Lichen planus
- · Porphyria cutanea tarda.
Laboratory features
- · ALT may be raised
- · Autoantibodies in serum
- · Anti-LKM.
Chronic hepatitis C Treatment
- IFN ex subcutaneous – 3 times a week for 6 months.
- IFN ex plus Ribavirin daily.
- Pegylated IFNs – Long acting IFN bound to polyethylene glycol (PEG) – have a longer half life with once weekly dose.
Chronic Autoimmune Hepatitis
- It is a chronic hepatitis with continued hepatocellular necrosis with fibrosis progressing to cirrhosis and liver failure.
- Mortality is high.
- Clinical features are similar to chronic viral hepatitis. Onset may be insidious or abrupt.
- Common in young or middle-aged women.
- There is high titer of circulating ANA
- There is fatigue, malaise, anorexia, amenorrhoea, acne, arthralgias, jaundice, arthritis, colitis, pericarditis, anaemia, sicca syndrome, cirrhosis.
- Course is variable. There may be hepatocellular carcinoma as a late complication.
Laboratory features
- · Serum AST 100 to 1000 units
- · Serum bilirubin normal to 10 mgjdL
- · Prothrombin time prolonged
- · Hypergammaglobulinemia >2.5 gjdL
- · ANA positive
- · Smooth- muscle antibodies
- · Anti-LKM 1 antibody.
Autoimmune Hepatitis Treatment
- Glucocorticoid therapy Cyclosporine Tacrolimus.