Article Contents ::
- 1 Chronic Renal Failure (CRF) OR CRD/CKD
- 2 Stages of Chronic Renal Disease/Chronic Kidney Disease (CKD)
- 3 Risk factors for CRD/CKD
- 4 History of CRF
- 5 Common causes of chronic renal disease and presentations
- 6 Pregnancy Considerations in CRF
- 7 Physical Examination in Chronic Renal Failure (CRF)
- 8 Genetics of CRF —
- 9 Cockcroft-Gault Equation for creatinine clearance
- 10 UREMIA IN CRF
- 11 Fluid, Electrolyte and Acid Base Disturbance Sodium and water
- 12 Treatment
- 13 Potassium
- 14 Metabolic acidosis in CRF
- 15 Treatment of Hyperkalemia and Acidosis
- 16 Bone disease and Disorders of Calcium and Phosphate
- 17 Treatment
- 18 Cardiovascular abnormalities in CRF
- 19 Treatment
- 20 Hematological abnormalities Anaemia due to :
- 21 Treatment
- 22 Neuromuscular abnormalities in CRF
- 23 Gastrointestinal abnormalities in CRF
- 24 Endocrine and Metabolic disturbances
- 25 Dermatologic abnormalities
- 26 Management Treatment of CRD
- 27 Indications for Dialysis in CRF
- 28 Indications for Kidney transplantation in CRF
Chronic Renal Failure (CRF) OR CRD/CKD
Chronic renal disease is a destruction of nephrons of the kidneys due to several causes. The damage to renal structure and function is irr versib This results in uremia which leads to dysfunction of several organs. Chronic kidney disease (CKD) is defined as kidney damage or glomerular filtration rate (GFR) <60 mL/min/1.73 m2for >3 months. The destruction of kidney is a chronic process of more than 3 months.
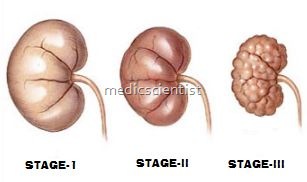
Stages of Chronic Renal Disease/Chronic Kidney Disease (CKD)
- Stage 1
- Kidney damage with normal or increased GFR – 90 ml/min/1.73 m2
- Stage 2
- Kidney damage with decreased GFR60-89
- Stage 3
- Moderately decreased GFR 30-59
- Stage 4
- Sftverely decreased GFR 15-29
- Stage 5
- Renal failure GFR < 15
Risk factors for CRD/CKD
- Family history of renal disease
- Hypertension
- Diabetes
- Autoimmune disease
- Old age
- History of acute renal failure
- Smoking
- Low income/education
- Ethnic minority status
- Evidence of kidney damage
- Proteinuria, abnormal urinary sediment, urinary tract structural abnormalities.
- A typical cause of chronic renal disease (CRD) is diabetic nephropathy.
- The first feature of CRD is usually albuminuria. Albumin-specific dipstick measurement of albumin to creatinine ratio in the first morning urine spot sample if more than 17 mg albumin per gram of serum creatinine in adult males and more than 25 mg albumin per gram of creatinine in adult females signifies CRD.
History of CRF
- Oliguria, nocturia, polyuria, change in urinary frequency
- Hematuria
- Bone disease
- Fatigue, depression, weakness
- Pruritus, tremor
- Metallic taste in mouth, uremia
- Anorexia, nausea, vomiting
- Obesity
- Dyspnea
- Hypertension
- Poorly controlled diabetes with retinopathy, neuropathy
- Hyperlipidemia
- Claudication
Common causes of chronic renal disease and presentations
- Diabetic kidney —>
- History of diabetes, proteinuria, retinopathy
- Hypertension —->
- High blood pressure, Family history, Normal urinary findings
- Non-diabetic glomerular disease —– >
- Nephritic, Nephrotic
- Cystic kidney disease —–>
- Urinary tract symptoms, abnormal urinary sediments, abnormal imaging findings
- Tubulointerstitial disease —–>
- UTI, Drugs, tubular syndromes, abnormal urine findings
Pregnancy Considerations in CRF
- Renal function in CKD may deteriorate during pregnancy.
- Creatinine >1.5 and hypertension are major risk factors for worsening renal function.
- Increased risk of premature labor, preeclampsia, and/or fetal loss
Physical Examination in Chronic Renal Failure (CRF)
- Complete physical plus ophthalmic exam; assess volume status (e.g., blood pressure with orthostatics; edema; jugular venous distention; weight)
- Skin: Sallow complexion, uremic “frost”
- Ammonialike odor (uremic fetor)
- Cardiovascular: Assess for mumurs, bruits, pericarditis
- At GFR (Glomerular Filtration Rate) less than 60 ml/ min all organ systems are affected.
- There is anaemia, loss of energy, decreasing appetite, abnormal calcium and phosphorus metabolism, metabolic bone disease, sodium, water, potassium and acid-base disturbances.
- At GFR < 15 ml/min the patient is not able to lead a regular life and may be in a uremic state needing’ urgent renal replacement therapy (dialysis etc.)
Genetics of CRF —
- There may be a monogenic inheritance,
- autosomal dominance or
- polymorphism of ACE (Angiotensin Converting Enzyme) genes.
Cockcroft-Gault Equation for creatinine clearance
- . Creatinine clearance ml/min in men = (140-age) X body weight in Kg. / 72 x Pcr mg/dl
- Creatinine clearance ml!min in women (140-age) X body weight in Kg. X 0.85 / 72 x Pcr mg/dl
UREMIA IN CRF
- Azotemia is retention of nitrogenous waste products due to renal insufficiency.
- Uremia is progressive renal insufficiency with multiorgan involvement.
- In uremia there is anorexia, malaise, vomiting, headache.
- In uremia there is toxicity due to urea, urates, hippurates, polyamines, phenols, benzoates and indoles.
- As a result there is :
- Anaemia Malnutrition
- Impaired metabolism of carbohydrates, fats and proteins
- Loss of energy Metabolic’ bone disease
- Increased levels of :
- PTH – parathyroid hormone
- Insulin ,
- Glucagon
- Luteinizing hormone
- Prolactin
- Decreased levels of :
- EPO – erythropoietin
- 1,25, dihydroxycholecalciferol
- Electrolyte abnormalities
Fluid, Electrolyte and Acid Base Disturbance Sodium and water
- There is increase of sodium and water in the body.
- There is sodium retention.
- There is extracellular fluid volume expansion (ECFV).
- Therefore, there is hypertension.
- There is weight gain.
- There is volume depletion only if there is vomiting, diarrhea, sweating, fever or diuretic administration.
Treatment
- Diuretics – loop diuretics, metolazone ‘Q/ Restricted salt intake
- Dialysis
- For volume depletion – normal saline infusion
Potassium
- There may be hypokalemia due to excretion of potassium in GIT.
- – There may be hyperkalemia due to constipation, protein catabolism, hemolysis, haemorrhage, RBC transfusion, metabolic acidosis.
- Drugs which may cause hyperkalemia are ACE inhibitors, ARBs, potassium sparing diuretics, Beta blockers and NSAIDs.
- hyperkalemia is more common in CRD than hypokalemia.
Metabolic acidosis in CRF
- ~There is metabolic acidosis because of reduced ability to produce ammonia.
- Hyperkalemia in CRD decreases ammonium excretion. This results in metabolic acidosis.
- In diabetics there is hyperkalemia, metabolic acidosis-renal tubular acidosis, hyporenin hypoaldosteronism.
- Treatment of hyperkalemia improves acidosis.
Treatment of Hyperkalemia and Acidosis
- Potassium binding resins
- Restriction of potassium salts
- Loop diuretics
- For acidosis NAHC03 may be given if pH <7.35 .
Bone disease and Disorders of Calcium and Phosphate
- High bone turnover and high PTH levels result in secondary hyperparathyroidism and osteitis fibrosa.
- Low bone turnover and low PTH level result in osteomalacia.
- Decreased GFR causes decreased excretion of phosphate and retention of phosphates.
- This causes increased PTH and lowering of calcium, decrease of calcitriol resulting in hypocalcemia and bone diseases, osteomalacia, vitamin D deficiency, metabolic acidosis.
- This causes bone pains, fractures, incapacity, difficulty in walking and movements.
- Calciphylaxis is metastatic calcification of soft tissue and blood vessels.
Treatment
- Calcitriol
- Avoid aluminium compounds Calcium acetate
- Calcium carbonate and Sodium phosphate binding agents.
Cardiovascular abnormalities in CRF
- Ischemic heart disease
- Hypertension
- Left ventricular hypertrophy
- Congestive heart failure Pulmonary edema
- Uremic pericarditis and cardiac tamponade, hemorrhagic pericardial effusion
- Dyslipidemias
- Hyperhomocysteinemia.
Treatment
- For hypertension:
- ACE I and ARB’s if serum creatinine less than three
- Nifedipine, hydralazine, diltiazem, minoxidil.
- For dyslipidemias :
- Statins, gemfibrozil
- For hyperhomocystinemia –
- Vitamins, folate supplementation
- Control of diabetes:
- Metformin is not used Insulin levels are increased in CRD
- For Pericarditis :
- Dialysis, pericardiectomy, aspiration of fluid.
Hematological abnormalities Anaemia due to :
- · Insufficient EPa (Erythropoietin)
- · Iron and folate deficiency
- · Hyperparathyroidism
- · Chronic inf~ction
- · Hemoglobinopathies
- · Coagulation abnormalities
- · Increased bleeding time
- · Increased platelet aggregation
- · Thromboembolic complications.
Treatment
- EPa (Erythropoietin) is given 50-150 units /kg/ week subcutaneous
- Side–effect of EPa – Hypertension, malignancies
- Iron supplementation Vitamin BI2, folate Anticoag u lant prophylaxis.
Neuromuscular abnormalities in CRF
- Central and Peripheral neuropathy Memory impairment
- Insomnia
- · Asterixis
- · Irritability
- · Muscle twitching
- · Seizures
- · Restless legs syndrome
- · Coma
Gastrointestinal abnormalities in CRF
- · Uremic fetor or odour or breath
- · Gastritis
- · Peptic disease
- · Abdominal pain, nausea, vomiting
- · Pancreatitis
- · Anorexia
- · Hiccups.
Endocrine and Metabolic disturbances
- · Impaired glucose metabolism
- · Plasma insulin levels are elevated
- · Amenorrhoea
- · Growth retardation.
Dermatologic abnormalities
- · Itching – Uremic pruritus
- · Pallor – Skin necrosis
Management Treatment of CRD
- · Control hypertension – ideal blood pressure 125/ 75
- · Control diabetes – preprandial glucose 90 – 130 mg/dl and HBA1C level <7.2%
- · Treat infections
- · Avoid nephrotoxic drugs
- · Estimation of plasma creatinine, GFR
- · Management of electrolyte imbalance
- · Management of acid-base disturbance
- · Ultrasound for kidney size, renal masses
- · Treat obstructive uropathy
- · Voiding cystourethrography and management
- · Renal biopsy and specific management
- · Management of bleeding
- · If kidney size <8.5 cm irreversibility of disease
- · Protein restriction to 0.6 g/kg/day
- · Dialysis
- · Kidney transplantation.
Indications for Dialysis in CRF
- Pericarditis
- Neuropathy due to uremia
- Encephalopathy
- Muscle irritability
- Anorexia, nausea, vomiting Fluid electrolyte abnormalities Severe volume overload Non-responsive hyperkalemia Progressive metabolic acidosis Asterixis
- Serum creatnine >8 mg/dl.
Indications for Kidney transplantation in CRF
- Irreversible ESRD (End Stage Renal Disease) Good antigenic match with donor
- First degree relative donor
- Primary transplantation.