Article Contents ::
- 1 Management of COPD
- 2 Diagnosis of COPD is considered in any patient with
- 3 Spirometry —
- 4 Chest X-ray for changes of COPD and other associated lesions.
- 5 Presence of respiratory failure and right heart failure indicates severe COPD.
- 6 Difference between COPD and Asthma
- 7 COPD —
- 8 Asthma —
- 9 MANAGEMENT OF COPD ACCORDING TO GOLD STAGING
- 10 DRUG MANAGEMENT BRONCHODILATOR MEDICATIONS
- 11 B2 agonists Short acting :
- 12 Anti-cholinergics
- 13 Inhaled glucocorticoids
- 14 Combination of long acting P2 agonists plus glucocorticoids
- 15 Systemic glucocorticoids
- 16 For acute episodes
- 17 Other Pharmacologic treatments
- 18 REHABILITATION for COPD
- 19 VENTILATORY SUPPORT In COPD
- 20 SUMMARY OF TREATMENT OF COPD
Management of COPD
- Assess and monitor the disease
- Prevention of risk factors
- Treatment of COPO
- Treatment of exacerbations
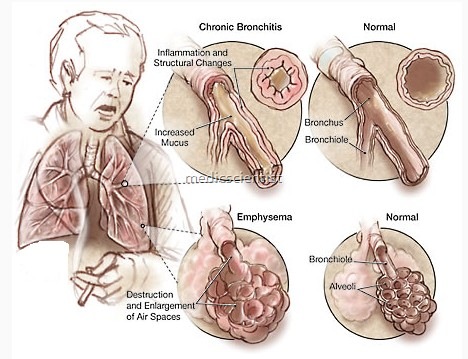
Diagnosis of COPD is considered in any patient with
- Chronic central cyanosis occurs in advanced stages of COPD and may be aggravated by exertion.
- Examination reveals wheezing and hyperresonant lung fields.
- cough,
- sputum production,
- dyspnoea and risk factors.
- Spirometry is done for airflow limitation.
- Barrel chest and clubbing are late signs.
- Tachycardia, diaphoresis, and flushing may also accompany COPD.
- Associated signs and symptoms include exertional dyspnea, a productive cough with thick sputum, anorexia, weight loss, pursed-lip breathing, tachypnea, and the use of accessory muscles.
Spirometry —
- Measure the maximal volume of air forcibly exhaled from the point of maximum inhalation (FVC – forced vital capacity).
- Measure volume of air exhaled during 1St second of the maneuver (forced expiratory volume in one second) – FEV1•
- Calculate ratio of FEV1/ FVC.
- Post bronchodilator FEV1 <80% of predicted value and FEV1/ FVC <70% is an airflow limitation which is not fully reversible.
Chest X-ray for changes of COPD and other associated lesions.
Presence of respiratory failure and right heart failure indicates severe COPD.
- Clinical signs of respiratory failure or right heart failure are central cyanosis, ankle swell~, and raised JV
- Respiratory failure is indicated by PaO2 <60 mmHg, PaCO2 >50 mmHg.
Difference between COPD and Asthma
COPD —
- Onset in middle life Symptoms slowly progressive Dyspnoea during exercise Long smoking history
- Family history variable
- Largely irreversible airflow limitation
Asthma —
- Onset in childhood
- Symptoms vary day to day Symptoms at night or early morning H/o allergy, rhinitis, eczema
- Family history of asthma
- Largely reversible airflow limitation
MANAGEMENT OF COPD ACCORDING TO GOLD STAGING
- Stage 0 – Avoidance of risk factors.
- Stage I – Avoidance of risk factors, short acting bronchodilators.
- Stage II – Avoidance of risk factors, short acting bronchodilators, long acting bronchodilators, rehabilitation.
- Stage III – Avoidance of risk factors, short acting bronchodilators, long acting bronchodilators, rehabilitation, inhaled glucocorticoids.
- Stage IV – Avoidance of risk factors, short acting bronchodilators; long acting bronchodilators, rehabilitation, inhaled glucocorticoids, plus long term oxygen if chronic respiratory failure, surgical treatment if required.
DRUG MANAGEMENT BRONCHODILATOR MEDICATIONS
-
B2 agonists Short acting :
- Salbutamol – Inhaler
- 100, 200 MOl (Metered Dose Inhaler) and DPI (Dry Powder Inhaler).
- 5 mg tab/cap 6-8 hrly, for oral use.
- Terbutaline – Inhaler 400, 500 DPI
- 2.5, 5 mg tablets 6-8 hrly, injection 0.2 mg vials.
- Long acting
- Formeterol inhaler – BD dose – 12 hrly
- Salmeterol inhaler – 12 hrly
-
Anti-cholinergics
- Short acting:
- or Ipratropium bromide inhaler – 8 hrly, Solution for nebulizer is also available.
- Long acting:
- Tiotropium – inhaler – OD – 24 hours dose. Combinations of short acting P2 agonists plus anticholinergics are available in inhalers.
- Methylxanthines Aminophylline
- 200 – 600 mg tab
- 240 mg vial for injection Theo hylline
- 100 – 600 mg tab., action up to 24 hours.
Inhaled glucocorticoids
- Beclomethasolle
- Budesonide
- Fluticasone
- Triamcinolone
Combination of long acting P2 agonists plus glucocorticoids
-
Systemic glucocorticoids
- Prednisone – 5 – 60 mg tab.
- Meth prednisolone – 4, 8, 16 mg tabs.
-
For acute episodes
- Nebulization with P2 agonists or anticholinergics is used.
- Regular glucocorticoid inhalers with long acting P2 agonists is useful for symptomatic COPD patients.
Other Pharmacologic treatments
- Vaccines – influenza and pneumococcal vaccine
- Alpha 1 anti-trypsin augmentation therapy
- Antibiotics
- Mucolytics – Ambroxol, Carbocysteine, Erdosteine
- Antioxidants – N- acetyl cysteine Immuno modulators Anti-tussives
- Narcotics
- Nedocromil, leukotrine modifiers.
REHABILITATION for COPD
- Patient Care: The respiratory therapist teaches breathing and coughing exercises and postural drainage to strengthen respiratory muscles and to mobilize secretions.
- The patient and family are assisted with disease-related lifestyle changes and are encouraged to express their feelings and concerns about the illness and its treatment.
- The patient is encouraged to participate in a pulmonary rehabilitation program, as well as to stop smoking and avoid other respiratory irritants.
- Frequent small meals and adequate fluid intake are encouraged.
- The patient’s schedule alternates periods of activity with rest.
- Patients are instructed to avoid contact with other persons with respiratory infections and taught the use of prescribed prophylactic antibiotics and bronchodilator therapy.
- · Exercise programs
- · Breathing exercises
- SURGICAL TREATMENTS Bullectomy (excision of bulla)
- , Lung volume reduction surgery
- • Lung transplantation
- Aerosolized bronchodilators are used to reduce dyspnea and promote improved cough.
- Low-concentration oxygen therapy is applied as needed to keep the PAo2 between 60 and 80 mm Hg.
VENTILATORY SUPPORT In COPD
- • For respiratory failure
- Non invasive intermittent positive pressure ventilation (NIPPV)
- Improves blood gases, reduces pH, reduces mortality.
- · NIPPV must be started if pH <7.35 i.e. severe acidosis, hypercapnia i.e. PaCo2 >45 mmHg and respiratory rate >25 breaths/ minute, severe dyspnoea.
SUMMARY OF TREATMENT OF COPD
- Anticholinergics and theophylline may be used in combination.
- For regular treatment, long-acting bronchodilators are better.
- Inhaled glucocorticosteroids + bronchodilators must be given if FEV1 <50% predicted i.e. severe CoPD.
- Exercise training program.
- Oxygen more than 15 hours per day in patients with chronic respiratory failure improves survival.