Article Contents ::
- 1 Tuberculosis Complete DRUGS –
- 2 History of treatment – Definitions for diagnosis:
- 3 ATT Abbreviations Tuberculosis :
- 4 Recommended Antituberculosis Treatment Regimens
- 5 RUGS – ATT (ANTITUBERCULAR TREATMENT) There are 3 main properties of antituberculous drugs:
- 6 Standard code for Anti- TB regimens :
- 7 treatment after interruption; treatment failure
- 8 TB treatment regimens
- 9 Chronic and MDR (Mutli-Drug Resistant) TB :
- 10 Management
- 11 Anti Tuburculous Drug Isoniazid
- 12 Rifampicin —
- 13 Pyrazinamide
- 14 Streptomycin It is bactericidal.
- 15 Ethambutol —
Tuberculosis Complete DRUGS –
- ATT (ANTITUBERCULAR TREATMENT) TREATMENT with Resistant and MDR Tubercular Treatment In All Cases
 |
| Complete RUGS – ATT (ANTITUBERCULAR TREATMENT) TREATMENT |
Case definitions:
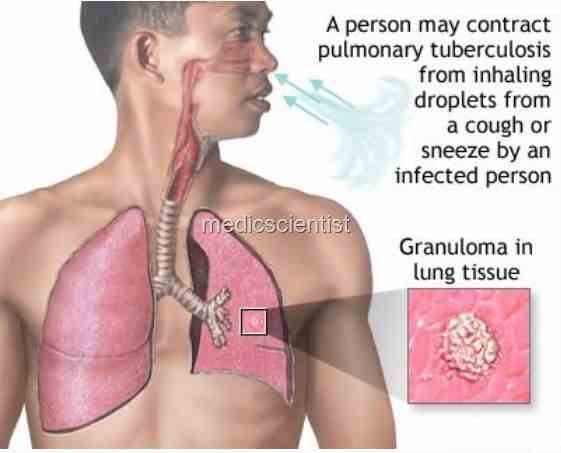
- 1. Tuberculosis suspect : Any person with symptoms or signs suggestive of tuberculosis like cough more than 2 weeks.
- 2. Case of tuberculosis: A patient in whom tuberculosis is confirmed bacteriologically
- 3. Definite case of tuberculosis : A patient with positive culture for M. tuberculosis complex or patient with 2 sputum smears showing AFB
| Complete RUGS – ATT (ANTITUBERCULAR TREATMENT) TREATMENT |
History of treatment – Definitions for diagnosis:
- 1. New -A patient who has never taken antitubercular treatment or taken for less than a month.
- 2. Relapse -A patient treated for TB and declared cured, or full treatment taken but smear or culture for tuberculosis is positive.
- 3. Treatment after failure – A patient given An again, after failed previous treatment
- 4. Treatment after default – If a patient, bacteriologically positive, interrupts treatment for 2 moths or more and starts An again.
- 5. Transfer in – A patient transferred from another TB centre for continuation of treatment.
- 6. Other – Any other case like chronic case, sputum positive at the end of repeat treatment.
- Sometimes pulmonary and extra pulmonary relapse cases may be smear-negative.
ATT Abbreviations Tuberculosis :
- H, isoniazid; R, rifampin; Z, pyrazinamide; E, ethambutol; S, streptomycin; Q, a quinolone antibiotic; PAS, para-aminosalicylic acid.
- aAll drugs can be given daily or intermittently (three times weekly throughout or twice weekly after 2–8 weeks of daily therapy during the initial phase).
- bStreptomycin can be used in place of ethambutol but is no longer considered to be a first-line drug by ATS/IDSA/CDC.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
- cThe continuation phase should be extended to 7 months for patients with cavitary pulmonary tuberculosis who remain sputum culture–positive after the initial phase of treatment.
- dHIV-negative patients with noncavitary pulmonary tuberculosis who have negative sputum AFB smears after the initial phase of treatment can be given once-weekly rifapentine/isoniazid in the continuation phase.
| Complete RUGS – ATT (ANTITUBERCULAR TREATMENT) TREATMENT |
RUGS – ATT (ANTITUBERCULAR TREATMENT) There are 3 main properties of antituberculous drugs:
- 1. Bactericidal action
- 2 Sterilizing activity
- 3-To prevent resistance.
The first line agents consist of Isoniazid, Rifampin, Pyrazinamide, Ethambutol.
- These drugs are given orally, once a day.
- Peak level is at 4 hours and effect lasts for 24 hours. Second line drugs have lower efficacy and more toxicity. These are streptomycin, kanamycin, amikacin, capreomycin, ethionamide, cycloserine, and PAS(Paraamino salicylic acid).
- Other drugs are Ofloxacin, Levofloxacin, Gatifloxacin, Moxifloxacin, Clofazimine, thiacetazone, amoxycillin and linezolid.
- Isoniazid and Rifampicin are strong bactericidal drugs. Pyrazinamide and streptomycin are also bactericidal Streptomycin is bactericidal against rapidly multiplying tubercle bacilli.
- Rifampicin is the most potent sterilizing drug. Ethambutol and thiocetazone prevent resistance to drugs.
Standard Treatment Regimens: Treatment is started with:
- 1 st– intensive phase for 2 months and
- 2 nd– continuation phase for 4 – 6 months.
Intensive phase consists of Isoniazid, Rifampicin, Pyrazinamide, and EthambutoL.
This intensive phase results in rapid killing of tubercle bacilli.
- In two weeks the infectious patient becomes noninfectious, symptoms subside.
- If patient is smear positive he becomes smear negative in two months.
Continuation phase consists of lesser drugs for longer time.
- This makes the patient disease-free and prevents resistance and relapse.
- Patients with large bacillary load (which means smearpositive or HIV-infected patients),’ are given short course chemotherapy with four drugs during initial phase and two drugs during continuation.
- Patients negative for HIV and smear negative tuberculosis are given rifampicin, isonex, pyrazinamide and ethambutol.
- Ethambutol may not be given in young children and primary tuberculosis.
Retreatment Regimen:
- For patients with smear or culture positive tuberculosis, 5 drugs in initial phase and 3 drugs in continuation phase should be given.
- Rifampicin, Isonex, Ethambutol are given throughout the treatment.
Standard code for Anti- TB regimens :
- Each antitubercular drug has an abbreviation as follows:
- Rifampicin – R
- Isoniazid – H
- Pyrazinamide – Z
- Streptomycin – S
- Ethambutol – E
- Thioacetazone – T.
Any regimen consists of :
- Initial phase
- Continuation phase
- The number before a phase is duration of that phase in months.
- Letters in brackets indicate the names of drugs.
- A subscript after the letters in brackets indicates number of doses per week. Eg. 2 (HRZE) / 4 (HR)3
- This means that initial phase of 2 months consists of Isoniazid, Rifampicin, Pyrazinamide, Ethambutol. The
TB Diagnostic TB Patients Category
- New smear positive patients; New smear negative PTB with extensive parenchymal involvement;
- Severe concomitant HIV disease or severe forms of EPTB
- Previously treated sputum smear-positive PTB :
- – relapse;
treatment after interruption; treatment failure
- New smear negative PTB (other than in Category I); Less severe forms of EPTB
- Chronic and MDR – TB cases (still sputum positive after supervised re-treatment)
Treatment Regimen in Special Conditions Pregnancy:
- Streptomycin is unsafe. It is hepatotoxic to fetus and so should not be used in pregnancy.
Breastfeeding :
- All drugs are safe. Baby can be given Isoniazid during infectious stage of mother and for 3 months after that.
Oral contraception:
- Rifampicin interacts with oral contraceptives and decreases their efficacy.
Liver disease:
- Isoniazid, Rifampicin and Pyrazinamide can cause hepatitis.
- Rifampicin is least toxic, but can cause cholestatic jaundice.
- Pyrazinamide is most hepatotoxic.
- Patients with chronic liver disease should not take Pyrazinamide.
- In chronic liver disease patient can take isoniazid and rifampicin with streptomycin and ethambutol for 8 months.
- In acute he(?atitis, treatment should be delayed till hepatitis resolves otherwise streptomycin and etham-
- continuation phase is of 4 months consisting of Isoniazid and Rifampicin given 3 times / week.
TB treatment regimens
- Initial phase (Daily Continuation phase
- or 3 times weekly) (Daily or 3 times weekly)a
- Specially designed standardized or individualized regimens are suggested for this category
- ethambutol can be given for 3 months and when hepatitis is resolved, isoniazid and rifampicin may be given.
- If acute hepatitis does not resolve for many months then only Streptomycin and Ethambutol should be continued for 12 months.
Renal Failure:
- In renal failure, Isoniazid, Rifampicin and Pyrazinamide can be given in normal doses.
- Pyridoxin should be given with Isoniazid to prevent peripheral neuropathy if renal failure patients.
- Streptomycin and Ethambutol are avoided or given in low doses.
- Thiocetazone should not be used.
- Patients with renal failure should be on 2 HRZ / 4 HR.
HIV infected patients:
- Thiocetazone is not given. Rest of the drugs can be given.
Chronic and MDR (Mutli-Drug Resistant) TB :
- Chronic tuberculosis is a patient with tuberculosis who. is sputum-positive after standard treatment with essential drugs given for complete duration.
- MDR TB is a patient who is Multi-Drug Resistant, i.e. who has active tuberculosis with bacilli resistant to at least Rifampicin and Isoniazid.
Minor
- Anorexia, nausea, abdominal pain Joint pains.
- Burning sensation in the feet
- Orange j red urine
- Pyrazinamide Isoniazid
Major
- Itching, skin rash Deafness (no wax on auroscopy) Dizziness (vertigo and nystagmus) Jaundice (other causes excluded) hepatitis
- Confusion (suspect drug induced acute liver failure if jaundice present)
- Visual impairment (other causes excluded)
- Shock, purpura, acute renal failure
- Thioacetazone (SHRZ) Streptomycin
- Isoniazid, Pyrazinamide, rifampicin
- Reserved drugs for tuberculosis are Amikacin, Kapriomycin, Ciprofloxacin, Cycloserine, Ethionamide, Kanamycin, Ofloxacin, p-aminosalycilic acid.
Management
- Continue anti-TB drugs, check drug doses Give drugs with small meals or last thing at night
- Aspirin
- Pyridoxine 100 mg daily
- Reassurance, Patients should be told when starting treatment that this commonly happens and is normal.
Stop responsible drug(s) Stop anti-TB drugs
- Stop streptomycin use ethambutol
- Stop anti-TB drugs
- Urgent liver function tests and prothrombin time
Management of Drug Induced Hepatitis:
- Isoniazid, Pyrazinamide, Rifampicin, and rarely Ethambutol can damage the liver.
- When a patient develops hepatitis during tubercular treatment, all An should be stopped till liver function tests become normal, or An is not given for 2 weeks after jaundice has disappeared. Rifampicin can give rise to jaundice without hepatitis and symptoms.
- For patients with drug-induced hepatitis Streptomycin, and Ethambutol may be given.
Anti Tuburculous Drug Isoniazid
- • Highly bactericidal
- · Given orally (1M also available)
- · Dose 5 mgjkg or 300 mgjday
- · Preventive dose 300 mgjday for 6 months
- · Contraindications – Active liver disease,
Hypersensitivity.
- In malnutrition, alcoholics, and diabetics, patient should be given pyridoxine 10 mgjday with Isoniazid.
Adverse Effects :
- Peripheral neu ropathy Optic neuritis
- Toxic psychosis Generalized convulsions Hepatitis.
Side effects :
- Nausea
- Vomiting Dizziness
- Blurred vision Slurring of speech Seizures.
Rifampicin —
- Strong bactericidal drug
- Should be given 30 minutes before meals Dose is 10 m k or 150 – 600 mg daily
- The drug causes red coloration of urine, tears, saliva, sweat, sputum and contact lenses. Contraindications:
- Hypersensitivity Liver dysfunction.
Adverse effects :
- Gastro-intestinal disturbances Fever
- Flu-like syndrome Thrombocytopenia Skin rashes Exfoliative dermatitis Oliguria
- Dyspnoea
- Hemolytic anaemia
- Hepatitis (which may be fatal).
Pyrazinamide
- Weak bactericidal, potent sterilizing activity. Dose – 30 mgLkgLQay.
Contraindications :
- Hypersensitivity Hepatic impairment.
Adverse effects :
- Gastrointestinal disturbances Increased serum transaminases Hyperuricemia
- Gout
- Arthralgia.
Streptomycin It is bactericidal.
- Given by deep intramuscular injection.
- Dose – 15 mg/kg/day or 750 mg – 1 gm /day. Contraindications :
- Hypersensitivity Auditory nerve deafness Myasthenia gravis
- Should not be used in pregnancy as it causes deafness and nephrotoxicity in the fetus.
Adverse effects :
- Injection abscess Hypersensitivity
- Impairment of vestibular function – Headache, vomiting, vertigo and tinnitus
- Nephrotoxicity
- Hemolytic anaemia
- Aplastic anaemia
- Agranulocytosis
- Thrombocytopenia
- Streptomycin should not be given to patients who are to receive neuromuscular blocking agents during anaesthesia.
Ethambutol —
- Its role is to prevent emergence of resistant strains. Dose – 15 mgLl<g/daL
Contraindication:
- . Hypersensitivity
- .• Optic neuritis
- Creatinine clearance < 50 ml/min.
Adverse effects :
- Optic neuritis – Visual impairment and loss of colour vision
- Blindness
- Peripheral neuritis

