Heart Failure
Heart failure is a state wherein the heart is unable to pump blood adequately to meet the needs of all the tissues and organs of the body at normal pressures.
Heart Failure Definition —
- Inability of the heart to circulate blood effectively enough to meet the body’s metabolic needs.
- Heart failure (HF) is a common clinical syndrome representing the end-stage of a number of different cardiac diseases.
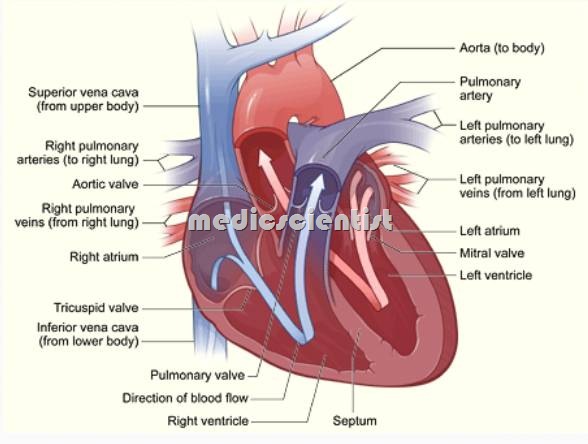
- Heart failure may affect the left ventricle, right ventricle, or both. It may result from impaired ejection of blood from the heart during systole or from impaired relaxation of the heart during diastole.
Heart failure is a syndrome with —
1. Symptoms at rest or during exercise:
- Breathlessness
- Fatigue
- Ankle swelling
2. Objective evidence of cardiac dysfunction:
- On clinical examination (tachycardia, cardiomegaly, left ventricular third heart soun9,sys 0 IC murmurs).
- Echocardiographic assessment –
- Other evidences
3. Heartfailur is also proved by the response to treatment.
Right and Left heart failure
- Right heart failure is a syndrgme presenting with congestion of systemic veins.
- Left heart failure is a s ndrome resenting witb congestion of ulmonar veins.
High and Low output failure
- High output failure – cardiac out ut is increased as in fever, thyrotoxicosis, pregnancy, physical stress, wet beri-beri(Thamine deficienc ), PDA, AR, MR etc.
- Usually high output States are Precipitating facrors for heart failure.
- AII chronic heart failures are usually low output failures, i.e. the cardiac output is low (there is heart muscle disease or pump failure). .
Acute Vs Chronic heart failure
- · Heart failure typically means a chronic state of decompensation
- · Acute heart failure means an acute exacerbation of chronic heart failure or acute decompensation of the diseased heart.
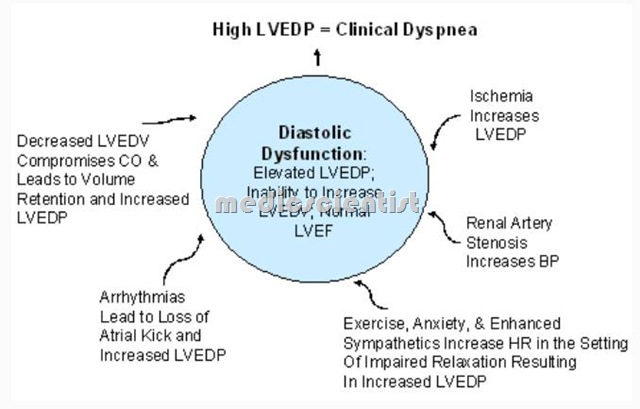
Systolic Vs Diastolic heart failure
- · In heart failure left ventricular systolic dysfunction is common.
- · Diastolic dysfunction is common in elderly but . uncommon in young patients.
Grades of heart failure
- Mild, Moderate or Severe heart failure are cli~cal descriptive terms.
- The NYHA (New York Heart Association) c1assifica ion of heart failure may be used for severity of heart failure with respect to any symptom of Heart Failure
- · Class I No limitation
- · Class II Slight limitation of activity
- · Class III Marked limitation of activity
- · Class IV Unable to carry out any physical activity without discomfort.
Stages in the development of HF —
- There are several stages in the evolution of HF, as outlined by the American College of Cardiology/American Heart Association (ACC/AHA) guidelines
- Stage A — High risk for HF, without structural heart disease or symptoms
- Stage B — Heart disease with asymptomatic left ventricular dysfunction
- Stage C — Prior or current symptoms of HF Stage D — Refractory end stage HF
Precipitating causes of heart failure
- · Infection
- · Arrhythmias
- · Stress
- · MI (Myocardial infarction)
- · Pulmonary embolism
- · Anaemia
- · Thyrotoxicosis
- · Pregnancy
- · HTN (Hypertension)
- · Myocarditis
- · Infective Endocarditis
Causes of Heart Failure
- · Cardiomyopathies
- · Viral myocarditis
- · HHD (Hypertensive heart disease)
- · Acute hypertensive crisis
- · Rupture of aortic valve reflect
- · Massive pulmonary embolism
- · Endocardial fibrosis
- · MI (Myocardial infarction)
- · IHD (Ischemic heart disease)
- · CHD (Congenital heart disease)
- · VHD (Valvular heart disease)
- · HOCM (Hypertrophic obstructive cardiomyopathy).
Symptoms and Signs Of Heart Failure —
- Difficulty breathing is the predominant symptom of heart failure.
- Breathlessness (dyspnoea) Ankle swelling
- PND (Paroxysmal nocturnal dyspnnoea) and orthopnea
- In patients with mild impairments of ejection fraction (e.g., 45% to 50%), breathing is normal at rest but labored after climbing a flight of stairs or lifting lightweight objects.
- Confusion, lack of concentration Impaired memory, insomnia, anxiety Headache
- Bilateral basal crepts and ronchi
- Decreased pulse pressure Increased diastolic blood pressure Reduced systolic blood pressure
- Patients with advanced heart failure (e.g., ejection fraction 20%) may have such difficulty breathing that getting out of bed or taking a few steps is very tiring.
- Anorexia, Nausea
- Nocturia
- Cheyne-Stokes respiration
- Splenomegaly
- Jaundice and Ascites
- Low volume pulse
- Acute pulmonary oedema
- Raised JVP (prominent neck veins) Fatigue
- Anasarca
- Hepatomegaly – tender, pulsating liver .,r Pulsus alternans
- sinus tachycardia
- Positive abdominojugular reflux 53, 54 audible – Gallop rhythm -yo MR, TR
- Cool diaphoretic extremities Cyanosis
- Pleural effusion
- Cardiac cachexia
- Pre-renal azotemia.
Paroxysmal Nocturnal Dyspnea
- Air hunger resulting in labored or difficult breathing, sometimes accompanied by pain. It is normal when due to vigorous work or athletic activity.
- It is also known as Cardiac Asthma.
- Sudden attacks of shortness of breath that usually occur when patients are asleep in bed.
- The affected patient awakens gasping for air and tries to sit up (often near a window) to relieve the symptom.
- There is severe breathlessness at night which awakens the patient from sleep.
- There is pulmonary congestion and increase of blood volume at night due to shift of edema fluid from the lower part of body during lying down.
- There is a feeling of suffocation and wheezing.
- During sleep the sympathetic drive is low and the diaphragm is pushed up towards the thorax.
- The patient therefore is severely short of breath and runs to the open window to inhale fresh air.
- When he gets relief he again lies down and goes to sleep.
- This is a typical attack of paroxysmal nocturnal dyspnea (PND).
Orthopnea in Heart Failure
- It is difficulty in breathing when lying down, so the patient sits up on the bed.
Cheyne-Stokes Respiration in Heart Failure
- It is cyclic or periodic respiration due to decreased response of respiratory’centre to Peor
- There is a phase of apnea when P02 falls and Peo2 rises followed by stimulation of respiratory centre resulting in hyperventilation again.
Heart Failure ECG
- · A normal ECG goes against the diagnosis of heart failure .
- · ECG may give a clue to the cause of heart failure and precipitating factor .
- · ECG of MI (myocardial infarction) and IHD (ischemic heart disease) common.
- · QRS width more than 120 ms in cardiac dyssynchrony.
Heart Failure X-ray
- · Clue to etiology
- · Cardiomegaly
- · Pulmonary congestion.
Lab tests in Heart Failure
- · CBC – Hb, TLC, DLC, platelets
- · S. electrolytes
- · S. glucose
- · S. creatinine
- · S. hepatic enzymes
- · Urine analysis
- · T3, T4, TSH
- · Troponins.
Heart Failure Natriuretic peptides
- BNP Brain natriuretic peptide) and NT-Pro BNP N terminal pro Brain natriuretic peptide are a ways elevated .
- Low BNP (Brain natriuretic peptide) levels rules out heart failure.
- Now available, affordable, cost-effective, timesaving, reliable.
Echocardiography of Heart Failure
- · Determine etiology
- · Ejection fraction
- · LV EDP (left ventricular end diastolic pressure)
- · Dimensions of cardiac chambers
- · To rule out Cardiomyopathy – dilated, restrictive, obstructive
Heart Failure Diagnosis of diastolic dysfunction
- · Signs and symptoms of CHF (congestive heart failure)
- Normal or mildly abnormal LVEF (Left ventricular ejection fraction) – >45%
- Impaired LV diastolic relaxation
- No pulmonary disease.
TEE (Trans-esophageal echocardiography) in Heart Failure
- · Not routinely
- · For thrombus in atrial appendage.
- · For mitral valve prosthesis
Other noninvasive tests for Heart Failure
- · Stress echo
- · Radionuclide imaging
- · CMR (Cardiac magnetic resonance) PFT (Pulmonary function test) Exercise stress test.
Invasive tests for Heart Failure
- Cardiac catheterization:
- · Coronary angiography
- · Ventriculography
- · Pulmonary artery catheterization.
Heart Failure Control
- · Hypertension
- · CAD (coronary artery disease)
- · Thyroid diseases
- · Obesity
- · Infections.
Treatment – General advice for Heart Failure
- · Education – counselling
- · Weight – gain and loss
- gain – >2 kg in 3 days is a warning loss – bad prognosis
- Diet – salt restriction
- Fluids – 1.5 to 2 L per day or less Alcohol – Restriction.
- Obesity – weight reduction Smoking – stopped
- Travelling – avoid high altitude, heat, humidity
Drugs – to avoid in Heart Failure
- NSAIDs (Non steroidal anti-inflammatory drugs) ClassI antiarrhythmics(ex.lidocaine, quinidine) CCBs (Calcium channel blockers)
- Tricyclic antidepressants
- Corticosteroids
- Lithium.
Heart Failure Patient care Rest and Exercise:
- . Rest – absolute bed rest for acute heart failure Exercise – to improve functional capacity, prevent venous thrombosis, improve skeletal muscle function.