Article Contents ::
- 1 ACUTE APPENDICITIS Symptoms Clinical Features Diagnosis Treatment
- 2 ACUTE APPENDICITIS
- 3 Etiology of APPENDICITIS
- 4 APPENDICITIS Pathophysiology
- 5 History for APPENDICITIS
- 6 Physical Exam for APPENDICITIS
- 7 APPENDICITIS Symptoms Clinical features
- 8 APPENDICITIS Diagnosis
- 9 Risk Factors in APPENDICITIS
- 10 Lab diagnosis
- 11 Imaging X-ray, CT,–
- 12 APPENDICITIS Treatment
- 13 Medication
- 14 Complications of APPENDICITIS
ACUTE APPENDICITIS Symptoms Clinical Features Diagnosis Treatment
ACUTE APPENDICITIS
Acute appendicitis is acute inflammation of the appendix.
- Acute appendicitis usually occurs in 2nd and 3rd decades in males and females equally.
- Perforation is common in infancy and elderly.
- appendicitis has been recognized as one of the most common causes of the acute abdomen worldwide,Classic presentations, which occur about 60% of the time, include abdominal pain (initially diffuse, gradually localizing to the right lower quadrant), loss of appetite, nausea, fever, and an elevated white blood cell count
- Acute inflammation of the vermiform appendix, 1st described by Reginald Fitz in 1886
- Most common cause of the acute surgical abdomen
Etiology of APPENDICITIS
- · Luminal obstruction, ulceration of mucosa, infection with Yersinia, fecoliths, enlarged lymphoid follicles, worms, tumors, may cause obstruction and appendicitis.
- · Ganwene and perforation may occur.
- Other foreign bodies
- Intestinal worms (ascarids)
- Strictures, fibrosis
- · Sometimes terminal ileum, cecum and omentum may adhe;re together and form a lump or abscess.
- · Appendicitis may also occur in Crohn’s disease.
- Fecaliths (most common)
- Lymphoid tissue hyperplasia (in children)
- Inspissated barium
- Vegetable, fruit seeds
- Neoplasms
APPENDICITIS Pathophysiology
- Acute obstruction raises intraluminal pressure, leading to ischemia.
- initial event to incite appendicitis is thought to be obstruction of the appendiceal lumen
- Bacteria invade the appendiceal wall at sites of ulceration, producing inflammation.
- Necrosis of appendiceal wall results in perforation with fecal contamination of the peritoneum.
History for APPENDICITIS
- Q: Is there constipation and inability to pass gas?
- A: These are considered traditional cardinal signs for irritation associated with peritoneal or abdominal mesentery.
- Q: Is there nausea or vomiting?
- A: Many surgeons feel that vomiting is the cardinal symptom associated with appendicitis.
- Q: Is there fever?
- A: Low-grade fever is common in appendicitis; higher fever can indicate an abscess or other infectious disease.
- Q: Does the pain move, or is there point tenderness associated in the right lower quadrant (RLQ)?
- A: Typically, there is poorly localized, cramplike mid-abdominal pain that migrates to the RLQ.
- Q: Other classic features?
- A: Rectal tenderness, nausea, anorexia; patient prefers to lie still; rarely, secretory diarrhea, more common in infants <2 years of age; change in bowel habits, especially diarrhea; guarding (i.e., voluntary contraction of the abdominal muscle); appendicitis may be presenting with unusual features.
- Toddlers are not able to explain the time of onset and localization of pain.
Physical Exam for APPENDICITIS
- Fever; temp >100.4°F (can be absent)
- Tachycardia
- Right lower quadrant (RLQ) tenderness
- Maximal tenderness at McBurney’s point
- Voluntary and involuntary guarding
- Cutaneous hyperesthesia at T10–12
- Rovsing sign: RLQ pain with palpation of LLQ
- Psoas sign: Pain with right thigh extension (retrocecal appendix)
- Obturator sign: Pain with internal rotation of flexed right thigh (pelvic appendix)
- Local and suprapubic pain on rectal exam (pelvic appendix)
- Pelvic and rectal exams necessary to explore other pathology (PID, prostatitis, etc.)
APPENDICITIS Symptoms Clinical features
- · Abdominal pain, usually in periumbilical or epigastric region.
- · Cramps, colics, lasting 4 to 6 hours.
- · Pain is aggravated by motion or cough, and is
- usually present in right lower quadrant later
- · Anorexia, nausea, vomiting.
- · Diarrhea.
- · Urinary frequency.
- · Tenderness in mid-abdomen and right lower
- quadrant.
- · Flexion of right hip due to local peritonitis.
- · Positive psoas or obturator sign.
- · Fever 99-100oF.
- · Tachycardia.
- · Rigidity and tenderness in diffuse peritonitis.
- · A mass may develop if there is perforation, in 3 days.
- · Mass is palpable in carcinoma of cecum.
APPENDICITIS Diagnosis
- The differential diagnosis of this presentation includes flares of inflammatory bowel disease, mesenteric adenitis, pelvic inflammation, and many other illnesses.
- Diagnosis is simple when pain eventually localizes to the right lower quadrant,
- with rebound tenderness and rigidity over the right rectus muscle or McBurney’s point.
Risk Factors in APPENDICITIS
- Infestation by Enterobius vermicularis or Ascaris lumbricoides
- Recent viral infection
- Adolescent males
- Familial tendency
- Intra-abdominal tumors
Lab diagnosis
- Urinanalysis to exclude urinary tract pathology
- CBC; elevated WBC count with left shift
- CRP; acute phase reactant, increased within 12 hours of onset of infection
- • Leucocytosis 10,000 to 18,000 per mm3
- · Anaemia and blood in stools
Imaging X-ray, CT,–
- · X-ray, CT, Ultrasound may show obstruction, calculus, mass, cysts, abscess etc.
- Abdominal x-ray:
- Air-fluid levels suggesting small bowel obstruction
- Indistinct psoas margins
- Often normal
- 8–10% show calcified fecalith
- Cecal wall thickening
- Pneumoperitoneum (rare)
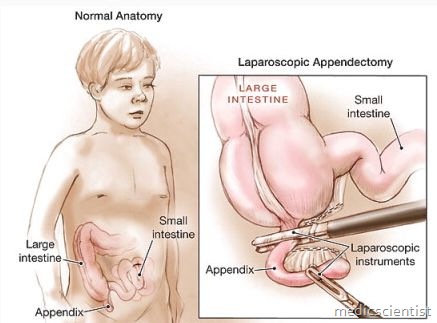
APPENDICITIS Treatment
- Avoid enema.
- Operative treatment, usually laparoscopic surgery.
- If there is palpable mass after 3 days, operation
- is not done. .
- Conservative treatment is antibiotics, fluids. Appendectomy is done 3 months later
Medication
First Line
- Uncomplicated acute appendicitis: 1 perioperative dose of broad-spectrum antibiotic
- Cefoxitin (Mefoxin); cefotetan (Cefotan)
- Gangrenous or perforating appendicitis:
- Broadened antibiotic coverage for aerobic and anaerobic enteric pathogens
- Fluoroquinolone and metronidazole typical
- Adjust dosage and choice of antibiotic based on intraoperative cultures
- Continue antibiotics for 7 days postoperatively or until patient becomes afebrile
Second Line
- Ampicillin-sulbactam (Unasyn)
- Ticarcillin-clavulanate (Timentin)
- Piperacillin-tazobactam (Zosyn)
- Surgery (appendectomy) is still the standard of care. However, nonoperative management with antibiotics has been studied as an alternative.
Complications of APPENDICITIS
- · Perforation; subphrenic, pelvic, intraabdominal abscess.
