Article Contents ::
- 1 HYPERSENSITIVITY PNEUMONITIS Clinical features Diagnosis and Treatment of Hypersensitivity
- 2 HYPERSENSITIVITY PNEUMONITIS (HP)
- 3 HYPERSENSITIVITY PNEUMONITIS History —
- 4 Chronic form: Develops after several months of exposure:
- 5 Subacute form: Develops after several days to weeks:
- 6 Other important points in history include:
- 7 Etiology of Hypersensitivity
- 8 Clinical features of Hypersensitivity
- 9 Diagnosis of Hypersensitivity
- 10 Lab Tests —
- 11 Chest x-ray
- 12 CT scanning
- 13 Pulmonary function test (PFT)
- 14 Treatment of Hypersensitivity
- 15 Corticosteroids
- 16 Contraindications : Refer to the manufacturer’s literature.
HYPERSENSITIVITY PNEUMONITIS Clinical features Diagnosis and Treatment of Hypersensitivity
HYPERSENSITIVITY PNEUMONITIS (HP)
- It is also called extrinsic allergic alveolitisis an inflammatory disease of alveolar walls, and terminal airways caused by repeated exposure to organic agents in a susceptible person.
- It’s also called farmer’s lung, commonly due to the HP caused by moldy hay.
- Usually the organisms responsible for the hypersensitivity reactions are Actinomyces, Micropolyspora faeni and Aspergillus.

HYPERSENSITIVITY PNEUMONITIS History —
- Acute form: Develops 2–9 hours following exposure
- Cough, dyspnea, fever, chills, diaphoresis, headache, nausea
- Symptoms last hours to days
Chronic form: Develops after several months of exposure:
- Progressively worsening cough and dyspnea
- Also develop fatigue, weight loss, anorexia
Subacute form: Develops after several days to weeks:
- Marked by worsening respiratory symptoms
Other important points in history include:
- History of pulmonary disease or recurrent infections
- Recent change in work or home
- Known exposure to pets, hot tubs, areas with water damage
- Symptomatic improvement when away from work or home
Etiology of Hypersensitivity
- · Different names are given to the different diseases depending on the occupation of host, the antigen’ exposed to, and the habit of the person.
- E.g. Farme(s lung due to moldy hay.
- · Chemical wo kers lung
- · Mushroom worker’s disease
- Bagassosis in sugarcane workers
- Wood workers’ lung.
- Humidity, temperature, concentration of antigen, duration of exposure and habits like smoking all increase the incidence of HP.
Clinical features of Hypersensitivity
- There is Lnterstitial pneumonitis.
- · Presentation may be acute, subacute or chronic.
- · Symptoms are cough, fever, dyspnoea, chills, malaise, from 6-8 hrs after exposure, to months from onset. Symptoms may persist for years.
- · In chronic form, there is pulmonary fibrosis, cyanosis, clubbing, pulmonary hypertension, respiratory failure and death.
- · On physical examination, there are bilateral basal crackles, reduced carbon monoxide diffusion capacity, and hypoxemia.
Diagnosis of Hypersensitivity
Lab Tests —
- •May have increased inflammatory markers (erythrocyte sedimentation rate, C-reactive protein)
- •Leukocytosis and increased gammaglobulins typically seen
- •Specific IgG antibody to offending agent can be detected and checked serially to detect response to treatment :
- Not always present (likely because many unknown antigens)
- Low specificity (10% of people exposed to farmer’s lung antigen develop antibodies; only 0.3% show symptoms)
- •Rheumatoid factor often positive (unknown cause)
- •Negative blood, sputum, throat cultures
- •Bronchoalveolar lavage (BAL)
- Acute form with neutrophils and CD4 T lymphocytes
- Chronic form with high number of CD8 T lymphocytes
- BAL may help to differentiate chronic hypersensitvity pneumonitis from sarcoid, which has high CD8 T lymphocytes
- -There is neutrophilia, lymphopenia, increased ESR, increased C reactive protein, rheumatoid factor, raised serum immunoglobulins.
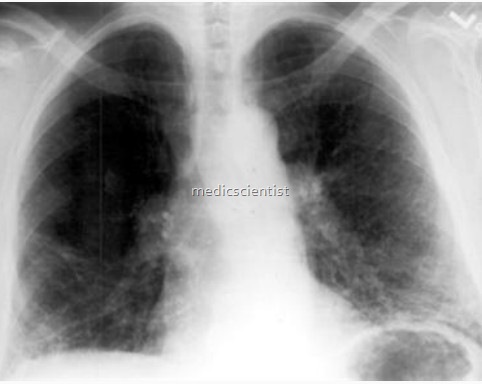
Chest x-ray
- Acute: Diffuse ground-glass infiltrates, nodular or striated patchy opacities. Up to 20% have normal CXR.
- Subacute: Same as acute, may have sparing of lung bases
- Chronic: Upper lobe fibrosis, reticular opacities, volume loss, honeycombing
- may be normal or show patchy or diffuse infiltrates or discrete nodular infiltrates. There may be honey-combing.
CT scanning
- is diagnostic showing the details of fibrosis, and nodules.
Pulmonary function test (PFT)
- shows a restrictive or obstructive pattern, decreased lung volume, impaired diffusion capacity, bronchial hyper reactivity and reversibility.
- BAL (Broncho alveolar lavage)
- shows lymphocytic alveolitis.
- Lung biopsy through bronchoscopy, may be diagnostic.
- Inhalation challenge i.e. a positive response to inhaled antigen may be done for transient airflow obstruction.
Treatment of Hypersensitivity
- The condition should be diagnosed by occupational history, lifestyle, livelihood, Hlo exposure to antigens .
- The exposure should be checked by wearing of appropriate masks, pollen masks, personal dust respirators, air helmets, ventilated helmets with fresh air.
- Glucocorticoids – Prednisone 1 mglkglday for 1-2 weeks tapered in 6 wks. Maintenance dose may be continued at the lowest possible dosage if symptoms recur.
- •Avoidance of offending antigen is primary therapy.
Corticosteroids
- Prednisone: 1–2 mg/kg/day, to max of 50–60 mg p.o. daily
- Initial course of 1–2 weeks with progressive taper
- Low-dose therapy (20 mg p.o. daily) may be as effective as avoidance.
Contraindications : Refer to the manufacturer’s literature.
- •Precautions: Observation for side effects:
- Acne
- Hirsutism
- Behavioral changes
- Immunosuppression
- Salt and water retention
- OsteoporosisWeight gain/appetite increase
