Article Contents ::
- 1 Pancreatitis (inflammatory disease of pancreas) Signs and Symptoms Diagnostic Tests
- 2 Pancreatic Diseases
- 3 Various presentations of Pancreatitis :
- 4 Pancreatitis Prognosis:
- 5 Pancreatitis Classic presentation
- 6 Pancreatitis Etiology
- 7 Pancreatitis Diagnostic Tests and Interpretation—
- 8 Lab
- 9 Other Tests
- 10 Tests for Pancreatic Structure X-ray: shows
- 11 Ultrasound: shows
- 12 CT is best for:
- 13 Endoscopic ultrasonography (EUS)
- 14 Magnetic Resonance Cholepancreatography (MRCP)
Pancreatitis (inflammatory disease of pancreas) Signs and Symptoms Diagnostic Tests
Pancreatic Diseases
Pancreatitis is inflammatory disease of pancreas
Various presentations of Pancreatitis :
- · Hypertriglyceridemia
- · Vitamin B12 malsorption
- · Hypercalcemia
- · Hypocalcemia
- · Hyperglycemia
- · Ascites
- · Pleural effusion
- · Chronic abdominal pain.
Pancreatitis Prognosis:
- Several techniques are used to determine how well (or how poorly) patients with pancreatitis will progress during their illness and whether they may benefit from intensive care.
- The best of these is the APACHE II system; it grades patients with pancreatitis on the basis of 14 measurable physiological parameters, including the patient’s
Pancreatitis Classic presentation
- Pancreatitis Signs and Symptoms
- Pancreatitis History
- •Similar to an acute abdomen of any cause
- •Acute pancreatitis:
- Alcohol use
- Past history of gallstones
- Family history of gallstones
- Medication use
- Abdominal trauma
- Recent weight loss
- •Chronic pancreatitis:
- Alcohol use
- Signs of steatorrhea
- Signs of hyperglycemia
- · Severe constant epigastric pain radiating to back.
- · Elevated serum amylase.
Pancreatitis Etiology
- · Unknown
- · Alcohol abuse
- · Biliary tract disease
- Drugs
- · Trauma
- · Viral infections
- · Metabolic and connective tissue disorders.
Pancreatitis Diagnostic Tests and Interpretation—
Lab
- •No test is 100% sensitive or specific
- •Acute pancreatitis:
- Elevated serum amylase (amylase P)
- Elevated serum lipase
- Liver function tests (LFTs): Hyperbilirubinemia and elevated (mild) ALT, AST, and/or alkaline phosphatase when associated with alcoholic hepatitis or choledocholithiasis
- Glucose increased in severe disease
- Calcium decreased in severe disease
- White blood cells (WBCs): 10,000–25,000/µL
Other Tests
- Serum Amylase: In patients with acute abdominal or back pain, estimation of serum amylase is done.
- If serum amylase is more than 65 units/litre, acute pancreatitis is a possibility.
- If serum amylase is more than 130 units per liter, the diagnosis is pancreatitis.
- In acute pancreatitis, serum amylase is increased from 24 hours to 3 days and returns to normal in 5 days.
- In acute pancreatitis, sometimes serum amylase may not be increased as in :
- 1. Late sample – after 5 days
- 2. In chronic pancreatitis
- 3. Hypertriglyceridemia.
- False elevation of serum amylase is seen in carcinoma lung, oesophagus, breast, ovary.
- Urinary amylase is not sensitive or specific. Elevation of pleural fluid and ascitic amylase occurs in other conditions also.
- Serum amylase more than 3 times normal is best test and highly specific for pancreatitis.
- Serum trypsinogen is elevated and is very specific for pancreas, but less sensitive.
- Normal is 28 to 58 ng/ml. Less than 20 ng/ml means> pancreatic steatorrhea.
- Trypsinogen levels are increased in pancreatitis as well as renal failure.
- Single best enzyme test for acute pancreatitis is lipase estimation.
Tests for Pancreatic Structure X-ray: shows
- 1. Localized ileus in jejunum (sentinel loop)
- 2. Generalized ileus with air fluid levels
- 3. Colon cut-off sign (isolated distension of trans-
- verse colon)
- 4. Duodenal distension with air fluid levels
- 5. Massive pseudocyst
- 6. In chronic pancreatitis – pancreatic calcification on and around second lumbar vertebra.
Ultrasound: shows
- · Edema
- · Inflammation
- · Calcification
- · Pseudocyst
- · Mass lesions
- · Gall stones.
- In acute pancreatfti~ pancreas is enlarged. Pancreatic pseudocyst – echo-free smooth round fluid collection.
- In pancreatic carcinoma – distortion of normal structures.
- If more than 3 cm localized echo-free solid lesion seen, it is usually carcinoma.
- In obesity and gas in large bowel, pancreas difficult· to see.
CT is best for:
- · Chronic pancreatitis and complications.
- · Pancreatic tumors
- · Pancreatic pseudocyst
- · Abscess
- · Calcium deposition.
- Dynamic CT using rapid IV contrast is for pancreatic necrosis to predict mortality and morbidity.
- Spiral CT is very good.
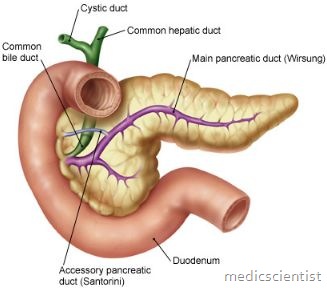
Endoscopic ultrasonography (EUS)
- is done to see pancreatic parenchyma and pancreatic duct, common bile duct stones, pseudo cyst.
- Endoscopic ultrasound (EUS) is better than Endoscopic retrograde cholepancreatography (ERCP).
- EUS is also for:
- Biopsy
- Nerve blocks through EUS Dilatation of main pancreatic duct.
Magnetic Resonance Cholepancreatography (MRCP)
- To see –
- Pancreatic duct Bile duct
- It is useful in elderly as it is a dure.
- Selective catheterization –
- of celiac and superior mesenteric arteries, and hepatic, splenic, and gastrgduodenal arteries for angiography.
- Percutaneous aspiration biopsy of pancreatic mass is done to differentiate between inflammatory swelli’ng and neoplasm.
- Exocrine pancreatic function
- 1. Direct stimulation of pancreas by IV infusion of secretin, or secretin plus CCK (cholecystokinin), then measurement of duodenal contents.
- 2. Study of digestion products from lumen like undigested meat fibers, stool fat, fecal nitrogen.
- 3. Measurement of pancreatic enzymes like elastase.
