Article Contents ::
- 1 Systemic Lupus Erythematosus (SLE) Diagnosis Symptoms and Treatment
- 2 Systemic Lupus Erythematosus (SLE)
- 3 SLE Clinical features Symptoms —
- 4 SLE History
- 5 SLE Physical Exam
- 6 SLE Pathogenesis
- 7 SLE Clinical manifestations Symptoms
- 8 DLE (Diffuse lupus erythematosus)
- 9 SLE Renal manifestations
- 10 Lab diagnosis:
- 11 I cular s ste
- 12 SLE Diagnosis
- 13 ELISA tests
- 14 Diagnostic Procedures
- 15 SLE Pulmonary and cardiac manifestations
- 16 SLE Gastrointestinal system
- 17 Ocular manifestations Retinal vasculitis:
- 18 Pregnancy and SLE
- 19 Bad Signs
- 20 Pregnancy and SLE Treatment
Systemic Lupus Erythematosus (SLE) Diagnosis Symptoms and Treatment
Systemic Lupus Erythematosus (SLE)
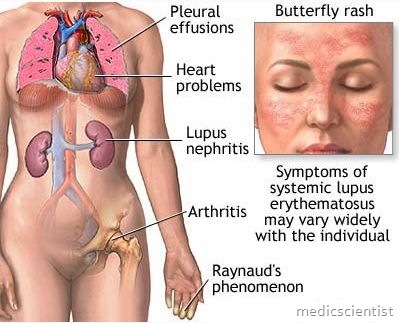
Systemic Lupus Erythematosus (SLE) is an autoimmune disease of unknown etiology in which there is tissue damage by pathogenic antibodies. Multisystem autoimmune inflammatory disease characterized by fluctuating, chronic course; varies from mild to severe and may be life-threatening (CNS and renal forms) chronic autoimmune inflammatory disease involving multiple organ systems and marked by periodic acute episodes. System(s) affected: Mucocutaneous; Musculoskeletal; Renal; Nervous; Pulmonary; Cardiac; Hematologic; Vascular, GI Its name is derived from the characteristic erythematous “butterfly” rash over the nose and cheeks, which resembles a wolf’s snout. Synonym(s): SLE, lupus
SLE Clinical features Symptoms —
SLE History
- Fever, fatigue, malaise, weight loss
- Rash, photosensitivity, alopecia
- Oral or nasal ulcers (usually painless)
- Arthritis, arthralgia, myalgia, weakness
- Pleuritic chest pain, cough, dyspnea, hemoptysis
- Headaches, visual deficits, stroke, seizure, psychosis, cognitive deficits
- Abdominal pain, anorexia, nausea, vomiting
- Raynaud phenomenon
- Recurrent pregnancy loss
SLE Physical Exam
- Vital signs: Fever, hypertension
- Malar rash, discoid rash, psoriasiform or annular rash, alopecia
- Oral or nasal ulcers
- Lymphadenopathy, splenomegaly
- Acrocyanosis
- Inflammatory arthritis, tenosynovitis
- Pleural or pericardial rub, heart murmur
- Bibasilar rales
- Cranial or peripheral neuropathies, retinopathy
- · Unknown etiology
- · Tissue damage by pathogenic antibodies
- · Autoimmune disease
- · Onset may be from one organ system
- · Autoantibodies detectable at onset.
- · Remission seen only in 20%
- · 90% cases are women (young)
- · Any age can be affected
- · More common in blacks.
SLE Pathogenesis
- Tissue damage by autoantibodies and immune complexes depends on :
- 1. T and B Iymphocyte hyperactivity
- 2. Susceptible genes
- Genetic marker is – Class HI allele C4AQO.
SLE Clinical manifestations Symptoms
- · Fatigue
- · Malaise
- Fever
- Anorexia
- Weight loss Arthralgias Myalgias, myopathy Arthritis
- – Severe pain and swelling in joints-hands,
- wrists, knees affected.
- Puffiness, tenosynontis, swan-neck deformities in 10%.
- Sub-cutaneous nodules.
- · Myopathy due to : – Hypokalemia
- – Glucocorticoids
- – Hydroxychloroquine.
- · Ischemic necrosis of bone – hip, knee, shoulder pain due to glucocorticoids.
- · Skin: Butterfly rash, photosensitive, fixed erythematous (red) rash, over cheeks, bridge of nose, ears and chin ·even.
- Sometimes diffuse maculopapular rash, sunburns. There is no scarring and loss of hair.
DLE (Diffuse lupus erythematosus)
- · DLE in 20% of patients
- · DLE is disfiguring
- · There is central atrophy and scarring of lesions
- · There is loss of hair
- · Occurs over scalp, ears, face, arms, back, chest (exposed areas only).
Less frequently Urtcaria Bullae Erythema multiforme Lichen planus Panniculitis. SLE SCLE (Subacute cutaneous lupus erythematous) Vasculitic skin lesions seen in SLE, DLE or SCLE.
- · Purpura
- · Sic nodule
- · Nail-fold infarcts
- · Ulcers
- · Vascular urticaria
- · Gangrene.
- Ulcers in nose and mouth in SLE.
SLE Renal manifestations
- Immunoglobulin (Ig) depositions in glomeruli. Clinical nephritis in 50%. There is proteinuria. Features of Nephrotic syndrome may be present:
- · Edema
- · Hematuria
- · Cylindruria
- · Proteinuria.
- Focal lesions, diffuse disease and It may progress to renal failure.
- SLE Renal biopsy: should be done if no response to :
- · Steroids
- · Cytotoxic drugs.
- If there is a high proportion of sclerotic glomeruli then treatment is by dialysis and renal transplant.
- SLE Risk of severe nephritis if :
- · Abnormal urine analyses
- · High titer of anti dsNA (double standard DNA)
- · Hypocomplimentemia.
e OUS!i S em
- There is involvement of : – Meninges
- – Spinal cord
- – Cranial and peripheral nerves.
- Some of the presentations are
- · Cognitive dysfunction
- · Headache
- · Seizures
- · Psychosis
- · Confusion
- · Demyelinating disorders
- · Cerebrovascular disease
- · Movement disorders
- · Aseptic meningitis
- · Myelopathy
- · Mono-polyneuropathy (GB syndrome)
- · Mood disturbance
- · Optic neuritis
- · Subarachnoid haemorrhage
- · Pseudotumor cerebri
- · Inappropriate secretion of vasopressin
- · Depression, anxiety.
Lab diagnosis:
- Abnormal EEG CSF (cerebro spinal fluid) :
- Increased protein levels Increased monocyte Increased Ig.
- Lumbar puncture / CSF not routine. MRI can diagnose focal lesion.
- CT Scan for detection of mass or haemorrhage. Angiograms for vasculitis, and occlusions and emboli
- Treatment
- Immunosuppressives Recurrence in 1/3 of patients.
I cular s ste
- Antibody against phospholipids
- · Lupus anticoagulants (LA)
- · Anticardiolipin (aCL).
- Lesions of Libman Sacks endocarditis may embolize to brain.
- Degenerative cerebral and coronary artery disease. Hyperlipidemia is side effect of long term steroid therapy
- Treatment:
- Anticoagulation, with or without immunosuppression.
- Manifestations
- · Anaemia
- · Hemolysis : +ve Coomb’s test Treatment
- – High dose Glucocorticoids, Splenectomy for refractory cases.
- · Leukopenia (No treatment)
- · Thrombocytopenia – Bleeding, Purpura Treatment
- – Steroids in high dose.
- – IV Gamma globulin gives short term response.
- – Addition of cytotoxic drugs after 2 weeks.
- – If no response: Cyclosporin, Danazole, Splenectomy.
SLE Diagnosis
- Russell viper venom tincture for LA (LUpus anticoagulants).
-
ELISA tests
- Lupus anticoagulants in
- · Thrombocytopenia
- · Recurrent arterial clotting
- · Recurrent venous clotting
- · Recurrent fetal loss
- · Valvular heart disease
- · Bleeding
-
Diagnostic Procedures
- Renal biopsy to diagnose lupus nephritis
- Skin biopsy with immunofluorescence on both involved and uninvolved non-sun-exposed skin (lupus band test) may help to differentiate SLE rash from other disorders.
- Lumbar puncture in patients with fever and CNS or meningeal symptoms
- EEG for seizures or global CNS dysfunction
- Neuropsychiatric testing for cognitive impairment
- EMG/NCS to diagnose peripheral neuropathy and myositis
- Nerve and/or muscle biopsy
- ECG, cardiac enzymes, stress tests
- Treatment:
- glucocorticoids for bleeding
SLE Pulmonary and cardiac manifestations
- • Pericarditis
- · Pericardial effusion, tamponade, constrictive pericarditis, myocarditis
- · AR (aortic regurgitation)/ MR (mitral regurgitation)
- · Libman Sacks endocarditis
- · Myocardial infarction
- · Vasculitis
- · Pleural effusion
- · Pneumonia – Fever, Dyspnea, Cough
- X-ray – Atelectasis, infiltrates, fibrosis
- · Pulmonary hypertension
- · Massive alveolar haemorrhage
- · ARDS.
SLE Gastrointestinal system
- · Nausea
- · Diarrhoea
- · Intestinal vasculitis Abdominal pain – Cramps
- – Vomiting
- – Diarrhoea.
- · Intestinal perforation
- · Intestinal obstruction
- · Acute Pane eatitis.
- Surgery avoided if X-ray shows – dilated loops.
- Treatment –
- Steroids.
Ocular manifestations Retinal vasculitis:
- · Sicca syndrome
- · Conjunctivitis
- · Episcleritis
- · Optic neuritis.
- Lab diag osis of SLE Screening test
- · ANAs (non specific) (Anti-nuclear anti bodies) – >95% patients +ve (non specific)
- – (High serum ANA)
- · dsDNA (Double stranded DNA)
- · Decreased complement
- · Urine analysis:
- – Hematuria. casts and protein
- · Serum creatinine increased.
Pregnancy and SLE
- · H/o repeated abortions
- · Give low dose heparin 5000 U sic BD
- · Low dose aspirin may be given
- · Low dose corticosteroids may be given
- · Disease may flare up in 6th week postpartum
- Neonatal lupus –
- may have skin rash and congenital permanent heart block.
- Survival in SLE is <75% at 20 years.
Bad Signs
- · Increased serum creatinine >1.4 mg/dl
- · Hypertension
- · Anaemia
- · Nephrotic syndrome
- · Hypoalbuminemia
- · Hypocomplementemia
- · Thrombocytopenia
- · Thromboembolic events.
Pregnancy and SLE Treatment
- No cure Glucocorticoids
- NSAIDs (cox 2 inhibitors)
- Antimalarials – 400 mg HCQ for few weeks (needs regular eye checkup)
- Intralesional steroids
- Oral dihydroepiandrosterone
- High dose steroids 1-2 mg/kg per day (QID) a tapered
- 3-5 days of methylprednisolone 1000 mg Look for steroid side effects
- Treat infections
- Calcium
- Vitamin D
- HRT – Hormone replacement therapy with estrogen
- Calcitonin.
- Cytotoxic agents
- Azathioprin Methotrexate Clorambucil Cyclophospha mide
- Plasmapharesis
- Anticoagulation –
- for Antiphospholipid syndrome .
- Cyclosporin
- Intravenous immunoglobulins Autologous stem cell transplantation