Article Contents ::
- 1 Acute Renal Failure (ARF)
- 2 ARF (Acute renal failure) is characterized by :
- 3 ARF may be of 3 types:
- 4 PRERENAL ARF
- 5 Hepatorenal syndrome
- 6 INTRINSIC RENAL ARF
- 7 Common causes of intrinsic ARF
- 8 Acute tubular necrosis
- 9 POST RENAL ARF
- 10 MAJOR CAUSES OF ARF PRERENAL
- 11 Renal Causes of ARF
- 12 Pathophysiology
- 13 FEATURES TO DIFFERENTIATE ACUTE AND CHRONIC RENAL FAILURE ARF
- 14 Clinical features of ARF
- 15 Interstitial nephritis suggested by
- 16 Urinary obstruction suggested by –
- 17 Prostate enlargement suggested by
- 18 Acute tubular necrosis (ATN) i.e. Ischemic ARF, Nephrotoxic ARF
- 19 BLOOD
- 20 ULTRASOUND
- 21 PYELOGRAPHY –
- 22 COMPLICATIONS
- 23 Causes of Hypocalcemia in ARF
- 24 TREATMENT OF ARF
Acute Renal Failure (ARF)
Acute renal failure due to intratubular crystal precipitation can be seen in a variety of clinical settings, the most common being acute uric acid nephropathy Acute renal failure (ARF) is defined as a sudden decrease of normal kidney function that compromises the normal renal regulation of fluid, electrolyte, and acid–base homeostasis.
ARF (Acute renal failure) is characterized by :
- · Decrease in GFR (reversible).
- · Retention of nitrogenous wastes.
- · Disturbance of balance of fluid volume, electrolytes and acid-base.
- Oliguria: Urine output <0.5 mL/kg/h in infants or <500 mL/1.73 m2/d in older children
- Anuria: Total cessation of urinary output
- Polyuria: Urine output >2 L/m2/d in infants and children or 3 L/d in adults
- ·Oliguria – i.e. urine output <400 ml/day.
- Pre-renal and post-renal failure may be reversible by prompt and appropriate treatment.
- ARF is usually asymptomatic. It is diagnosed by a recent increase in blood urea and creatinine.
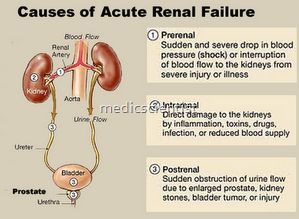
ARF may be of 3 types:
- 1. Prerenal
- 2. Renal
- 3. Post renal.
- Pre-renal –
- There is renal hypoperfusion. Renal parenchyma is normal.
- Renal –
- Renal parenchymal disease is present.
- Post renal –
- There is urinary tract obstruction leading to renal failure.
- ARF is mostly reversible.
PRERENAL ARF
- It is reversible by proper perfusion of kidneys so that glomerular ultrafiltration pressure becomes normal. Renal parenchymal tissue is normal.
- If tissue hypoperfusion persists there is damage of renal parenchyma.
- Due to hypoperfusion there is :
- Activation of sympathetic nervous system.
- Activation of renin angiotensin – aldosterone system .
- Release of AVP / ADH (arginine vasopressin / antidiuretic hormone).
- Norepinephrine, angiotensin II and AVP cause vasoconstriction in non-essential areas, inhibit salt loss through sweat glands, stimulate thirst, promote salt and water retention.
- Prostaglandin E2and prostacyclin cause dilatation of afferent arterioles.
- Angiotensin II causes preferential constriction of efferent arterioles.
- Thus glomerular filtration pressure is increased and glomerular filtration rate is increased.
- All these processes help to counter the renal hypoperfusion.
- GFR (Glomerular filtration rate) is maintained only if systemic pressure is above 80 mmHg.
Hepatorenal syndrome
- In advanced cirrhosis and other liver diseases there is severe form of ARF, called hepatorenal syndrome.
- Mortality is very high.
INTRINSIC RENAL ARF
- This may be due to :
- 1. Disease of larger renal vessels
- 2. Disease of glomeruli
- 3. Ischemic and nephrotoxic ARF
- 4. Tubulointerstitial disease.
Common causes of intrinsic ARF
- · Ischemia (Acute tubular necrosis)
- · Nephrotoxins.
Acute tubular necrosis
- Acute tubular necrosis or Ischemic ARF occurs in trauma, haemorrhage, sepsis, volume depletion. It can occur on preexisting renal disease.
POST RENAL ARF
- Post renal ARF is usually due to obstructive causes and are fully reversible with surgical treatment .
MAJOR CAUSES OF ARF PRERENAL
- Haemorrhage
- Burns
- Dehydration
- Vomiting and diarrhea
- Diabetes mellitus (osmotic diuresis)
- Pancreatitis Peritonitis
- Hypoalbuminemia
- Low cardiac output Pulmonary hypertension Sepsis
- Anti hypertensives
- Norepinephrine Epinephrine
- Cirrhosis and ascites (Hepatorenal)
- ACE inhibitors
- Multiple meyloma.
Renal Causes of ARF
- Renal artery obstruction by thrombus, embolism Renal vein thrombosis
- Glomerulonephritis
- Vasculitis
- Thrombotic thrombocytopeniac purpura Toxaemia of pregnancy
- DIC (Disseminated intravascular coagulation) SLE (Systemic lupus erythematosus) Scleroderma
- Acute tubular necrosis (Ischemia or hypoperfusi6n)
- Toxins
- PPH (Post Partum Haemorrhage) Abruptio placentae
- Drugs Cyclosporin
- Antibiotics
- NSAIDs
- Radiocontrast dye
- Interstitial nephritis Infections.
- Calculi Cancer
- Clot
- Stricture Bladder neck obstruction
- Urethral obstruction.
Pathophysiology
- ARF is commonly precipitated by an ischemic or nephrotoxic event.
- Initial vasodilatation is followed by intense vasoconstriction, with blood redistributed from the cortex to the juxtamedullary nephrons
- Intratubular debris and cast formation develop.
- Tubular fluid leaks backward across the injured tubular membrane, which, in addition to tubular obstruction, causes further hemodynamic changes.
FEATURES TO DIFFERENTIATE ACUTE AND CHRONIC RENAL FAILURE ARF
- Recent increase in urea and creatinine.
- There is history suggestive of the cause of ARF like diarrhoea, vomiting, burns etc.
- CRF
- Anaemia Neuropathy
- Rena I osteodystrophy Small, scarred kidneys
- Kidney size may be increased or normal in CRF due to :
- Diabetic nephropathy Amyloidosis
- Polycystic kidney disease
- Usually the kidney size is reduced in CRF .
Clinical features of ARF
- Thirst
- Orthostatic hypotension
- Systemic hypotension (BP <90 mmHg) –v Tachycardia (Pulse rate >100 Imin)
- Tachypnoea
- Raised JVP
- Dry skin and mucous membrane
- Reduced sweating
- History of NSAIDs, ACE-I (ACE inhibitors), ARBs
- (Angiotensin receptor blockers) v Decreased urine output
- Decreased body weig ht
- Hypovolemia
- Sepsis
- Hlo Radiocontrast dye
- Flank pain
- Atheroembolization suggested by Sic nodules, ischemia of fingers, toes
- Glomerulonephritis suggested by oliguria, edema, hypertension, active urine sediment.
Interstitial nephritis suggested by
- Fever,
- arthralgias,
- pruritic (that itch) red rash.
Urinary obstruction suggested by –
- Colicky pain
- Suprapubic and flank pain
- oFlank pain – loin tropain.
Prostate enlargement suggested by
- Nocturia
- Frequency
- Hesitancy.
URINE
- Oliguria or Anuria.
Prerenal ARF
- · Urine is acellular
- · Inactive sediments or hyaline casts present.
Post renal ARF
- · Inactive sediment
- · Hematuria
- · Pyuria.
Acute tubular necrosis (ATN) i.e. Ischemic ARF, Nephrotoxic ARF
- · Pigmented, muddy brown granular casts with tubule epithelial cells in urine.
- · Mild proteinuria « 19/day
Glomerular involvement
- Tubulointerstitial disease – RBC casts in urine.
Interstitial nephritis
- · WBC casts in urine.
- · Nonpigmented granular casts in urine.
Chronic renal disease
- Broad granufar casts in urine.
- Eosinophils -in urine – allergic interstitial nephritis. Uric a~id crystal~ in – acute urate nephropathy.
Proteinuria >1g/day suggests gIomerular disease. Heavy proteinuria> 1 g/day also seen in patients on NSAIDs, ampicillin, rifampicin, interferon alpha. Bilirubin in urine in hepatorenal syndrome. Fractional excretion of sodium
- FE Na < 1 % in prerenal ARF
- FE Na > 1 % in ischemic, nephrotoxic (tubular disease).
BLOOD
- Serum creatinine: increases progressively in renal failure and is a very good indicator of renal failure.
- Hyperkalemia
- Hyperphosphatemia
- Hypocalcemia
- Hyperuricemia
- Anaemia
ULTRASOUND
- Ultrasonography is useful for post renal ARF to diagnose causes like – urinary tract obstruction, pelvicalyceal dilatation, retroperitoneal fibrosis, neoplasia.
CT, MRI PLAIN X-RAY ABDOMEN
- For nephrolithiasis.
PYELOGRAPHY –
retrograde, antegrade –
- for localization of site of obstruction.
- For patency of renal arteries and veins.
MR ANGIOGRAPHY
- Non-invasive renal vascular study. CONTRAST ANGIOGRAPHY
RENAL BIOPSY –
- For definitive diagnosis.
- For intrinsic renal ARF e.g. glomerulonephritis, vasculitis, thrombocytopenic purpura, interstitial nephritis.
COMPLICATIONS
- There is impairment of renal excretion of sodiurtl, potassium and water.
- · Volume overload
- · Raised JVP
- · Hyponatrem ia
- · Hyperkalemia
- · Hyperphosphatemia
- · Hypocakemia
- · Hypermagnesemia
- · Metabolic acidosis
- · Uremia
- · Weight gain
- · Basal lung rales
- · Dependent edema
- · Pulmonary edema
- · Cerebral edema
- · Seizures
- · Arrhythmias
- · Metabolic acidosis
- · Lactic acidosis
- · Hemolysis
- · Leucocytosis
- · GI bleeding and bleeding from other sites
- · Infections
- MI
- Pericarditis Pericat”dial effusion Pulmonary embolism Uremic syndrome.
Causes of Hypocalcemia in ARF
- Metastatic deposition of calcium phosphate when the serum calcium X phosphate in mgjdl is > 70.
- Tissue resistance to parathyroid hormone. Decreased 1,25 dihydroxyvitamin D.
Effects of hypocalcemia
- Muscle cramps Seizures Hallucinations Confusion
- Prolonged QT.
TREATMENT OF ARF
- Prevention of pre-renal and post-renal causes Avoid drugs causing ARF
- Low drug dosage of nephrotoxic drugs Maintain fluid balance
- Maintain sodium, potassium, phosphate, calcium levels
- Invasive and noninvasive hemodynamic monitoring
- Low dose dopamine
- Loop diuretics (frusemide, torsemide) Antihyperte~sives like CCB (Calcium channel blockers) and Alpha-blockers
- Atrial natriuretic peptide
- Prostaglandins
- Antioxidants Glucocorticoids Alkylating agents Plasmapharesis
- Relief of obstruction of urinary tract
- Oral or IV sodium bicarbonate if arterial pH <7.2 or serum bicarbonate < 15 meq/L
- Restriction of dietary phosphate
- Oral aluminum hydroxide
- Calcium carbonate
- Vitamin D
- Restriction of dietary protein 0.6 g/kg/day Carbohydrate 100 g/day
- Blood transfusion if required
- Rarely erythropoietin for anemia
- Antacids
- PPI (proton pump inhibitor) and H2blockers Anti biotics
- Dialysis – if hemodynamically unstable peritoneal dialysis is done
- Hemodialysis – in uremic syndrome, refractory hyperkalemia, acidosis
- Continuous renal replacement therapy (CRRT) Continuous arteriovenous hemodiafiltration (CAVHD)
- Continuous venovenous hemodiafiltration (CVVHD).