Article Contents ::
- 1 APH (Antepartum Haemorrhage) and Placenta previa (PP) Diagnosis Symptoms
- 2 APH (Antepartum haemorrhage)
- 3 Cause of APH
- 4 Placenta previa (PP)
- 5 APH Epidemiology
- 6 Other risk factors
- 7 APH Etiology
- 8 Cause of bleeding
- 9 Clinical Manifestations symptoms —
- 10 APH Diagnosis
- 11 Examination.
- 12 Laboratory Studies
- 13 Complications
APH (Antepartum Haemorrhage) and Placenta previa (PP) Diagnosis Symptoms
APH (Antepartum Haemorrhage) and Placenta previa (PP) APH (Antepartum Haemorrhage)
- } It is defined as bleeding from or into the Genital tract.
APH (Antepartum haemorrhage)
Cause of APH
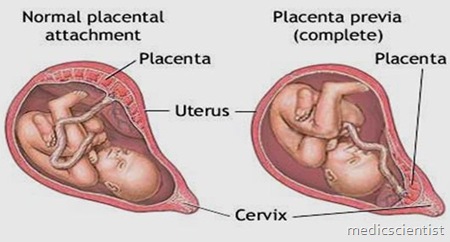
} I. Placenta previa (PP) is defined as the presence of placental tissue over or near the internal cervical os. } PP can be classified into four types based on the location of the placenta relative to the cervical os: to the internal os.
Placenta previa (PP)
- } Type-1/low-lying placenta,
- ◦ placenta is located near (2 to 3 cm) but not directly adjacent
- } Type-2/marginal previa,
- ◦ the edge of the placenta lies adjacent to the internal os;
- } Type-3/partial previa,
- ◦ the margin of the placenta covers part but not all of the internal os;
- } Type-4/complete or total previa,
- ◦ the placenta covers the entire cervical os;
- } 1. the incidence of PP is 1 in 200 to 1 in 390 pregnancies over 20 weeks’ gestational age).
- ◦ varies with parity,
- ◦ For nulliparous, the incidence is 0.2%, in grand multiparous, it may be as high as 5%
- } 2. The most important risk factor for PP is a previous cesarean section.
- ◦ PP occurs in 1% of pregnancies after a cesarean section.
- ◦ The incidence after four or more cs increases to 10%
APH Epidemiology
- ◦ increasing maternal age after age 40),
- ◦ multiple gestation, and previous uterine curettage
- ◦ the placenta covers the cervical os in 5% of pregnancies when examined at midpregnancy.
- ◦ The majority resolve as the uterus grows with gestational age.
- ◦ The upper third of the cervix develops into the lower uterine segment, and the placenta “migrates” away from the internal os.
Other risk factors
- } Unknown —
- ◦ a. Endometrial scarring.
- ◦ b. A reduction in uteroplacental oxygen promotes need for an increase in the placental surface area that favors previa formation.
APH Etiology
- } Bleeding occur in association with the development of the lower uterine segment in the third trimester.
- } Placental attachment is disrupted because this area gradually thins in preparation for labor.
- } the thinned lower uterine segment is
Cause of bleeding
- } unable to contract adequately to
- } prevent blood flow from the open vessels.shearing action
- } Vaginal examination or intercourse may also cause separation of the placenta from the uterine wall.
- } 80% of affected patients present with painless vaginal bleeding
- } Most commonly, the first episode is around 34 weeks of gestation;
- } one-third of patients develop bleeding before 30 weeks
- } Anaemia
Clinical Manifestations symptoms —
- } Abnormal growth of the placenta into the uterus can result in one of the following 3 complications:
- } i. Placenta Previa Accreta.
- } ii. Placenta Previa Increta.
- } iii. Placenta Previa Percreta.
- } 1. History.
- ◦ PP presents with acute onset of painless vaginal bleeding.
- ◦ A thorough history should be obtained from the patient, including obstetric and surgical history as well as documentation of previous ultrasound examinations.
- ◦ Other causes of vaginal bleeding must also be ruled out, such as placental abruption.
APH Diagnosis
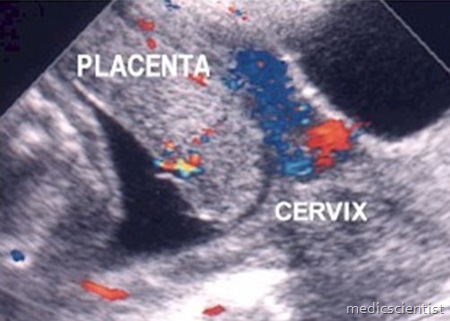
- } Vaginal sonography –
- ◦ is the gold standard for diagnosis of previa
- ◦ Placental tissue has to be overlying or within 2 cm of the internal cervical os to make the diagnosis.
- ◦ The diagnosis may be missed by transabdominal scan,
- ◦ if the placenta lies in the posterior portion empty bladder may help in identifying anterior previas, and Trendelenburg positioning may be useful in diagnosing posterior previas.
Complete placenta previa. Sagittal mid-line view of the lower uterus performed tau the placenta (PL) completely covering the cx Marginal/partial placenta previa in 3RD trimester patient with bleeding. Tvu shows inferior edge of posterior pl (P) located at internal CX os
- } If PP is present, digital examination is contraindicated.
- ◦ a. A speculum examination can be used to evaluate the presence and quantity of vaginal bleeding, the amount of vaginal bleeding can be assessed without placing a speculum and potentially causing more bleeding.
- ◦ b. Maternal vital signs, abdominal exam, uterine tone, and fetal heart rate monitoring should be evaluated.
Examination.
- } 4. . The following laboratory studies should be done for a patient with PP with vaginal bleeding:
- ◦ a. Complete blood cell count
- ◦ b. Type and cross-match
- ◦ c. Prothrombin time and activated thromboplastin time
- ◦ d. Kleihauer test to assess for fetomaternal hemorrhage
Laboratory Studies
- } Maternal—
- ◦ Anaemia with shock or CHF
- ◦ Malpresentation
- ◦ Premature labour
- ◦ Rarly rupture of membrain
- ◦ Post partum haemorrhage
- ◦ Sepsis
- ◦ subinvolution
Complications
- } Foetal complications include
- ◦ Low birthweight baby
- ◦ Asphyxia
- ◦ IUD
- ◦ Birth injury
- ◦ Congenital malformation
- } 1. Standard Management
- ◦ a. In the third trimester in a patient who is not bleeding, recommendations include
- } ultrasound confirmation
- ◦ pelvic rest (nothing in the vagina, including intercourse or pelvic exams),
- ◦ explanation of warning signs and when to seek immediate medical attention,
- ◦ avoidance of exercise and strenuous activity, and fetal growth ultrasounds every 3 to 4 weeks.
- ◦ Fetal testing semiweekly