Article Contents ::
- 1 Causes of Hemoglobinopathies Blood
- 2 Hemoglobinopathies
- 3 Classification of Hemoglobmopathies —
- 4 I. Structural hemoglobinopathies–
- 5 II. Thalassemia –
- 6 III. Thalassemic variants –
- 7 IV. HPFH –
- 8 V. Acquired hemoglobinopathies
- 9 Diagnosis of Hemoglobmopathies —
- 10 The SICkLE CELL SYNDROMES —
- 11 SICkLE CELL
- 12 Clinical manifestations of Hemoglobmopathies —
- 13 THALASSEMIA SYNDROMES —
- 14 THALASSEMIA
- 15 Clinical manifestations of thalssemia syndromes —
- 16 Clinical manifestations of thalssemia
- 17 Treatment of Hemoglobmopathies —
Causes of Hemoglobinopathies Blood
- disorders Syndromes Diagnosis Treatment —
 |
Hemoglobinopathies |
- Oxygen is delivered to tissues by hemoglobin. Hemoglobin is present in erythrocytes in high concentration and is responsible for the shape of the cell, viscosity of blood and cell deformability.
- Hemoglobinopathies are disorders of structure, function or production of hemoglobin.
- Different hemoglobins are produced during embryonic, fetal and adult life.
- The major adult hemoglobin HbA has the structure a2b2
- Minor adult hemoglobin is HbA2,a2d2
- HBF or fetal hemoglobin is —a2g2
- HbF predominates during gestation.
- During post natal life, only small amounts of HBF is present.
- At about 6 wks of gestation, the Hb is mainly embryonic Hb.
- At 10 – 11 weeks, HbF becomes predominant. At 38 wks most of the Hb is HbA.
- During stress, as in hemolytic anaemias, bone marrow transplant, chemotherapy, HbF increases.
- Hydroxyurea also increases HbF.
Classification of Hemoglobmopathies —
I. Structural hemoglobinopathies–
- 1. Sickle cell anaemia – HbS
- 2. Polycythemia, cyanosis
- 3. Hemolytic anaemia
- 4. Jaundice
- 5. Methemoglobinemia.
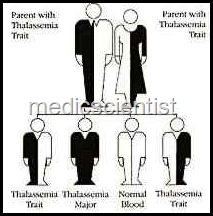
II. Thalassemia –
- Alpha thalassemia,
- Beta thalassemia,
- Alpha-beta thalassaemia.
III. Thalassemic variants –
- HbE thalassemia
- – Hb Lepore
IV. HPFH –
- Hereditary persistence of fetal hemoglobin in adult life.
V. Acquired hemoglobinopathies
- 1. Methemoglobinemia
- 2. Sulfhemoglobinemia
- 3. Carboxyhemoglobinemia.
Diagnosis of Hemoglobmopathies —
- is by haemoglobin electrophoresis and sickling tests.
The SICkLE CELL SYNDROMES —
 |
SICkLE CELL |
- These are hemoglobinopathies with abnormal hemoglobin HbS.
- The cells are sickle-shaped, non-pliable and therefore cause vascular occlusion. The cells are easily destroyed leading to hemolytic anaemia. The cells are rigid and cause occlusion of capillaries and veins causing tissue ischemia, pain, damage and infarction of organs.
- Sickle-cell anaemia is the homozygous state for HbS.
Clinical manifestations of Hemoglobmopathies —
- are anaemia, hemolysis, vascular occlusions, pain in limbs, renal failure, acute chest syndrome, chest pain, tachypnea, fever, cough, pulmonary embolization, cor-pulmonale.
- The most common clinical manifestation is recurrent acute pain, fever, and tachycardia called painful crises. Repeated crises more than 3 per year require hospitalisation and have bad prognosis.
- The spleen may disappear within 3 years of life due to repeated microinfarction.
- The hand-foot syndrome is due to painful infarct in the digits.
- Sickle cell trait is asymptomatic, because HbS/A is 60/40.
THALASSEMIA SYNDROMES —
 |
THALASSEMIA |
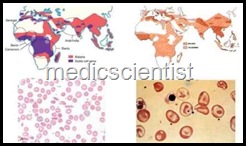
- These are inherited disorders of alpha or beta globin synthesis. There is hypochromia and microcytosis.
Clinical manifestations of thalssemia syndromes —
ody>
 |
Clinical manifestations of thalssemia |
- are deranged growth and development, anaemia, chipmunk facies with maxillary marrow hyperplasia, frontal bossing, thin long bones, growth retardation, hemolytic anaemia, hepatosplenomegaly, and congestive heart failure.
- Chronic transfusions with RBCs prolong life but iron overload occurs and death can occur in 3rd decade.
- Alpha thalassemia syndromes may be asymptomatic or have hemolytic anaemia.
- Patients of beta thalassemia minor and beta thalassemia trait are asymptomatic.
- Treatment consists of chronic blood and RBC transfusion, and splenectomy.
- Splenectomy is recommended if several transfusions are required in a year.
- Folic acid supplements and vaccination with pneumovax is done before splenectomy.
- Antenatal diagnosis is now widely available. PCR amplification of fetal DNA is used for specific diagnosis.
Treatment of Hemoglobmopathies —
- of sickle cell syndrome is analgesics, antibiotics, morphine, oxygen therapy, blood transfusion.
- Hydroxyure a 10 mg/kg/day increases fetal hemoglobin and is helpful.
- Other drugs are azacytidine and decitabine.
- Bone marrow transplantation is curative in children. Gene therapy may provide the best treatment.
This is short description about Hemoglobinopathies.
