Article Contents ::
- 1 Hyperbilirubinemia Classification Types Symptoms Examination
- 2 Hyperbilirubinemia
- 3 HISTORY AND PHYSICAL EXAMINATION —
- 4 Classification of jaundice according to type of bile pigment and mechanism
- 5 Unconjugated hyperbilirubinemia
- 6 Conjugated hyperbilirubinemia
- 7 Hemolytic jaundice
- 8 Ineffective erythropoiesis
- 9 Physiological Neonatal Jaundice
- 10 Crigler-Najjar Syndrome – Type I
- 11 Cngler Najjar Syndrome – Typ 11
- 12 Gilbert’s Syndrome
- 13 Dubio Johnson Syndrome
- 14 Rotor syndrome
- 15 Byler disease
Hyperbilirubinemia Classification Types Symptoms Examination
Hyperbilirubinemia
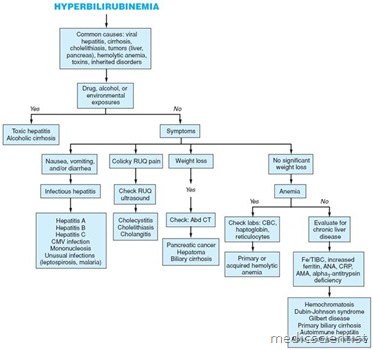
Hyperbilirubinemias are conditions where the serum bilirubin is high. An excessive amount of bilirubin in the blood; the condition is seen in any illness causing jaundice, including diseases in which the biliary tree is obstructed, and those in which blood formation is ineffective Pediatrics:In newborns, high bilirubin levels due to rapid destruction of red blood cells may be caused by maternal factors such as Rh or ABO incompatibility, prenatal use of certain therapeutic drugs, or intrauterine viral infection.
HISTORY AND PHYSICAL EXAMINATION —
- Multiple clues to the etiology can be obtained from the history,
- which should include the following information:
- Medications Use of drugs or herbal medications
- Use of alcohol Hepatitis risk factors
- History of abdominal operations, including gallbladder surgery
- History of inherited disorders including liver diseases and hemolytic disorders
- HIV status
- Travel history Exposure to toxic substances
Classification of jaundice according to type of bile pigment and mechanism
-
Unconjugated hyperbilirubinemia
- Increased bilirubin production*
- Extravascular hemolysis
- Extravasation of blood into tissues
- Intravascular hemolysis
- Dyserythropoiesis
- Impaired hepatic bilirubin uptake
- Congestive heart failure
- Portosystemic shunts
- Some patients with Gilbert’s syndrome
- Certain drugs – rifampin, probenecid flavaspadic acid, bunamiodyl
- Impaired bilirubin conjugation
- Crigler-Najjar syndrome type I and II
- Gilbert’s syndrome
- Neonates
- Hyperthyroidism
- Ethinyl estradiol
- Liver diseases – chronic persistent hepatitis, advanced cirrhosis, Wilson’s disease
-
Conjugated hyperbilirubinemia
- Extrahepatic cholestasis (biliary obstruction)
- Choledocholithiasis
- Intrinsic and extrinsic tumors – eg, cholangiocarcinoma
- Primary sclerosing cholangitis
- AIDS cholangiopathy
- Acute and chronic pancreatitis
- Strictures after invasive procedures
- Certain parasitic infections – eg, Ascaris lumbricoides, liver flukes
- Intrahepatic cholestasis
- Viral hepatitis
- Alcoholic hepatitis
- Nonalcoholic steatohepatitis
- Primary biliary cirrhosis
- Drugs and toxins – eg, alkylated steroids, chlorpromazine, herbal medications (eg, Jamaican bush tea), arsenic
- Sepsis and hypoperfusion states
- Infiltrative diseases – eg, amyloidosis, lymphoma, sarcoidosis, tuberculosis
- Total parenteral nutrition
- Postoperative patient
- Following organ transplantation
- Hepatic crisis in sickle cell disease
- Pregnancy
- End-stage liver disease
- Hepatocellular injury
* Serum bilirubin concentration usually less than 4 mg/dL (68 mmol/L) in the absence of underlying liver disease
Hemolytic jaundice
- Due to excess hemolysis there is unconjugated hyperbilirubinemia.
- Usually the serum bilirubin is less than 4 mgjdl.
- Common causes: viral hepatitis, cirrhosis, cholelithiasis, tumors (liver, pancreas), hemolytic anemia, toxins, inherited disorders
Ineffective erythropoiesis
- In Thalassemia major, megaloblastic anaemia, congenital erythropoietic porphyria, lead poisoning, and dyserythropoietic anaemias, bilirubin production is increased resulting in unconjugated bilirubinemia.
- In large hemat mas, massive infiuctions There may be unconjugated hyperbilirubinemia.
- In drug-induced cholecystographic contrast agent and novobiocin-induced jaundice there is unconjugated bilirubinemia.
Physiological Neonatal Jaundice
- Unconjugated hyperbilirubinemia is seen between 2nd and 5th day after birth. Jaundice may be up to 10 mgj dl. .~
Crigler-Najjar Syndrome – Type I
- There is defect in glucuronide conjugation of bilirubin and other substrates.
- There is unconjugated hyperbilirubinemia up to 45 mgjdl, with AST and ALT normal and no hemolysis. This is a rare disorder. There is often death due to kernicterus (bilirubin encephalopathy).
Cngler Najjar Syndrome – Typ 11
- In this also there is defective conjugation of bilirubin but bilirubin concentration is less than in eN-I. Marked unconjugated hyperbilirubinemia, with normal AST and ALT not associated with kernicterus (bilirubin encephalopathy) .
Gilbert’s Syndrome
- In this syndrome there is defect in bilirubin uptake and conjugation.
- There is mild unconjugated hyperbilirubinemia, serum bilirubin is less than 3 mgjdl.
- AST and ALT are normal.
- Gilbert syndrome is common with prevalence more than 8%, with male: female ratio 5 : 1.
Dubio Johnson Syndrome
- There is defective hepatic excretion of bilirubin.
- There is low grade conjugated hyperbilirubinemia. It is rare.
- ALT and AST are normal.
Rotor syndrome
- This is autosomal recessive disorder, with conjugated bilirubinemia, no jaundice and very rare.
- It is due to defective hepatobiliary function.
- The gall bladder is usually visualized on oral cholecystography whereas in DJS the gall bladder is not visualized.
Byler disease
- Presents in infancy with cholestatic jaundice.
