Article Contents ::
- 1 Bronchiectasis Signs and Symptoms Diagnosis Treatment
- 2 Bronchiectasis Signs and Symptoms
- 3 Bronchiectasis Pathology
- 4 Risk Factors for Bronchiectasis
- 5 Bronchiectasis Etiology
- 6 Physical examination of Bronchiectasis
- 7 Diagnostic Tests & InterpretationBronchiectasis
- 8 Differential Diagnosiswith Bronchiectasis
- 9 Treatment of Bronchiectasis
Bronchiectasis Signs and Symptoms Diagnosis Treatment
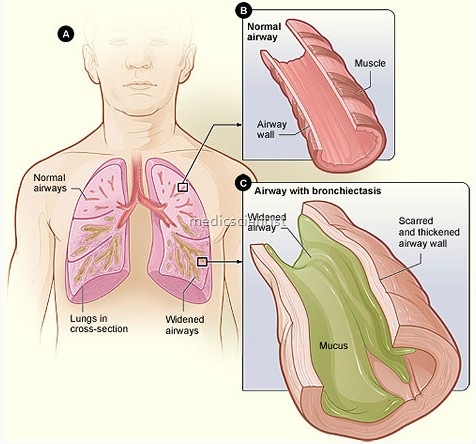
Bronchiectasis is an abnormal and permanent dilatation of bronchi. It may be focal or diffuse. Bronchiectasis is an irreversible dilation of one or more airways accompanied by recurrent transmural bronchial infection/inflammation and chronic mucopurulent sputum production. Generally classified into cystic fibrosis (CF) and noncystic fibrosis (non-CF) bronchiectasis. Chronic dilation of a bronchus or bronchi, usually in the lower portions of the lung, caused by the damaging effects of a long-standing infection.
Bronchiectasis Signs and Symptoms
- Chronic cough,
- sputum production,
- dyspnea, and
- wheezing are common.
Bronchiectasis Pathology
- The cartilage, muscle, elastic tissue of the wall of the bronchi are destroyed and replaced by fibrous tissue.
- Cylindrical bronchiectasis – the bronchi are uniformly dilated.
- Varicose bronchiectasis – Irregular dilatations of bronchi.
- Saccular bronc:;hiectasis – ballooning at the end of bronchi.
Risk Factors for Bronchiectasis
- Nontuberculous mycobacterial infection is both a cause and complication of non-CF bronchiectasis
- Severe respiratory infection in childhood (measles, adenovirus, influenza, pertussis, or bronchiolitis)
- Systemic diseases (e.g., rheumatoid arthritis and connective tissue disorders)
- Chronic rhinosinusitis
- Recurrent pneumonia
- Aspirated foreign body
- Immunodeficiency
Bronchiectasis Etiology
- The condition may be acquired or congenital and may occur in one or both lungs.
- Acquired bronchiectasis usually occurs secondary to an obstruction or an infection such as bronchopneumonia, chronic bronchitis, tuberculosis, cystic fibrosis, or whooping cough.
- Tuberculosis
- Pseudomonas aeruginosa infection
- Hemophilus influenzae
- Adenovirus
- Influenza virus
- Staphylococcus aureus
- Klebsiella
- HIV
- Mycoplasma and fungal infection
- Kartagener’s syndrome
- Cystic fibrosis
- Carcinoid tumors
- Foreign bodies
- Allergic bronchopulmonary aspergillosis
- Alpha 1 antitrypsin deficiency
- Ulcerative colitis Rheumatoid arthritis
- Sjogren’s syndrome
- Ammonia toxicity.
- CF bronchiectasis: Bronchiectasis due to cystic fibrosis
- Non-CF bronchiectasis:
- Most cases are idiopathic
- The etiologic agent most commonly associated with non-CF bronchiectasis is a childhood respiratory infection
- May be associated with many conditions
Physical examination of Bronchiectasis
- Chronic cough (90%)
- Sputum may be copious and purulent (90%)
- Rhinosinusitis (60–70%)
- Fatigue may be a dominant symptom (70%)
- Dyspnea (75%)
- Chest pain may be pleuritic (20–30%)
- Hemoptysis (20–30%)
- Wheezing (20%)
- Bibasal crackles (60%)
- Rhonchi (44%)
- Digital clubbing (3%)
- reveals
- Crackles,
- rhonchi, wheezes
- Clubbing
- Cor-pulmonale
- RVF.
Diagnostic Tests & InterpretationBronchiectasis
- Chest CT: Increased production of mucopurulent phlegm and dilated and thickened airways on CT should raise clinical suspicion
- Spirometry:
- Limited use in diagnosis
- Characterized by moderate airflow obstruction and hyper-responsive airways FEV1 <80% predicted and FEV1/FVC <0.7
- Special tests:
- Ciliary biopsy by electron microscopy
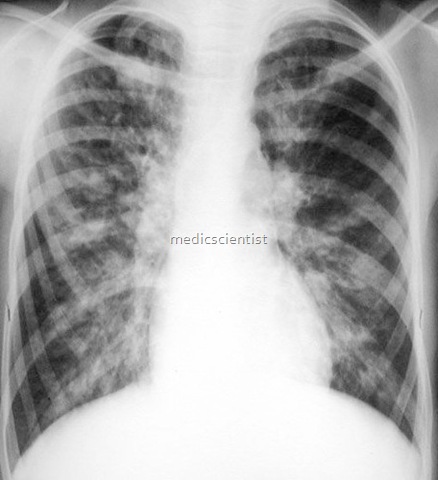
- X-ray
- Chest radiograph:
- Nonspecific findings; sensitivity and specificity are too low to confirm the diagnosis
- Increased lung markings
- May appear normal
- May be normal.
- May show cystic spaces, air-liquid levels, dilated. airwa s, hone -combin , atelectasis, tram tracks and ring shadows, prominent bronchial markings.
- Bronchography
- Not very useful.
- CT Scan
- High resolution CT demonstrates bronchiectasis very clearly.
- Noncontrast high-resolution chest CT is the most important diagnostic tool Bronchi are dilated and do not taper; varicose constrictions and balloon cysts may also be appreciated
- Sputum examination
- For organisms – culture and sensitivity.
- Fiberoptic bronchoscopy
Differential Diagnosiswith Bronchiectasis
- Chronic obstructive pulmonary disease
- Asthma
- CF
- Chronic bronchitis
- Pulmonary TB
- Allergic bronchopulmonary aspergillosis
Treatment of Bronchiectasis
- Useful in acute exacerbations
- Chronic therapy decreases sputum volume and purulence, but does not diminish the frequency of exacerbations
- Patients may require twice the usual dose and may require a longer course of treatment (7–14 days)
- Sputum culture and sensitivity should be used to direct therapy, as antibiotic selection is complicated by the wide range of culprit pathogens and the existence of resistant organisms
- Identify the problem
- Drainage of secretions – postural drainage and
- suction
- Mucolytics
- Control infections
- Management of airflow.
- Should be administered IV in cases of severe infection:
- Augmentin — 500 mg PO q.8–12 h for 7–10 days. Pediatric: Base dosing on amoxicillin content
- Trimethoprim/sulfamethoxazole : 160 mg TMP/800 mg SMX PO q.12 h for 10–14 days.
- Pediatric: 2 months, 8 mg/kg TMP and 40 mg/kg SMX PO per 24 hours, administered in 2 divided doses q.12 h for 10 days.
- Doxycycline and cefaclor given orally are also effective
- Nebulized aminoglycosides (tobramycin): 300 mg by aerosol b.i.d.
- Macrolides: Appear to have immunomodulatory benefits
- CYSTIC FIBROSIS
- This disease is characterized by chronic airways infection with bronchiectasis, bronchial ectasis, exocrine pancreatic insufficiency, intestinal dysfunction, abnormal sweat gland function, urogenital dysfunction .
- There is primary ciliary dyskinesia situs inversus sinusitis and broncheactasis.