Article Contents ::
- 1 Portal Hypertension Clinical Features Symptoms Diagnosis and Treatment
- 2 Portal Hypertension
- 3 Increased resistance can occur at :
- 4 Obstruction in presinusoidal veins may be :
- 5 Sinusoidal obstruction –
- 6 Post sinusoidal obstruction
- 7 Portal vein obstruction
- 8 Classification of noncirrhotic portal hypertension
- 9 Portal Hypertension Clinical Features Symptoms
- 10 Portal Hypertension Diagnosis
- 11 Portal Hypertension Treatment
Portal Hypertension Clinical Features Symptoms Diagnosis and Treatment
Portal Hypertension
- Normal pressure in portal vein is 5-10 mmHg. Vascular resistance in hepatic sinusoids is low.
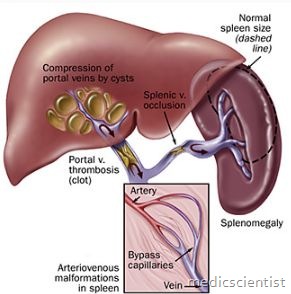
Increased pressure in the portal vein caused by an obstruction of the flow of blood through the liver. Portal hypertension is found in diseases such as cirrhosis, Portal hypertension is defined by a pathological increase in the pressure of the portal venous system. Portal hypertension means pressure in portal vein >10 mmHg.
- It results from increased resistance to blood flow due to any cause.
- in which it is responsible for ascites, splenomegaly, and the formation of varices.
- There are no valves in the portal venous system, therefore, any resistance from the right side of heart to the vessels of any organ results in direct transmission of the raised pressure.
Increased resistance can occur at :
- 1. Presinusoidal
- 2. Sinusoidal
- 3. Postsinusoidal levels. ,
Obstruction in presinusoidal veins may be :
- Outside the liver – portal vein thrombosis.
- Inside the liver – capillaries and venules.
Sinusoidal obstruction –
- In cirrhosis the increased resistance is sinusoidal.
Post sinusoidal obstruction
- may occur outside the liver.
- . In the hepatic veins – Budd Chiari syndrome.
- · In the inferior vena cava.
- · Within the liver – Veno-occlusive disease.
- Functional resistance to portal blood flow may occur at several levels.
- Portal hypertension may also occur in massive splenomegaly or AV fistulas due to increased blood flow.
- The most common cause of portal hypertension is cirrhosis of liver.
- Portal hypertension is present in more than 60% of cirrhosis patients.
Portal vein obstruction
- is the next common cause and may be :
- · Idiopathic – due to hypercoagulable states like polycythemia vera, essential thrombocythemia, protein C, protein S and antithrombin III deficiencies.
- · Cirrhosis
- · Infection
- · Pancreatitis
- · Abdominal trauma.
- Portal vein occlusion may result in hematamesis from oesophageal varices and ascites.
Non–cirrhotic portal hypertension is rare.
Classification of noncirrhotic portal hypertension
- Prehepatic
- Portal vein thrombosis Splenic vein thombosis Splanchnic arteriovenous fistula Splenomegaly (lymphoma, Gaucher’s disease)
- Intrahepatic
- Presinusoidal Schistosomiasis Idiopathic portal hypertension/Noncirrhotic portal fibrosis/Hepatoportal sclerosis Primary biliary cirrhosis Sarcoidosis Congenital hepatic fibrosis Sclerosing cholangitis Hepatic arteriopetal fistula
- Sinusoidal Arsenic poisoning Vinyl chloride toxicity Vitamin A toxicity Nodular regenerative hyperplasia
- Postsinusoidal Sinusoidal obstruction syndrome (Veno-occlusive disease) Budd-Chiari syndrome
- Posthepatic
- IVC obstruction Cardiac disease (constrictive pericarditis, restrictive cardiomyopathy)
Portal Hypertension Clinical Features Symptoms
- · Oesophageal variceal bleeding
- · Splenomegaly with hypersplenism
- · Ascites
- · Acute and chronic hepatic encephalopathy.
- There is development of portal systemic collaterals. There is retrograde flow away from the liver from high pressure portal venous system to low pressure systemic venous circulation.
- Major collaterals are oesophageal varices, rectal, retroperitoneal, periumbilical or abdominal wall collaterals.
- On the abdomen, collaterals appear as tortuous epigastric vessels radiating from umbilicus upwards, the caput medusae. There is a progressive reduction in platelet count.
- A low platelet count may be the first clue to cirrhosis. ,
- A marked fall in platelets and WBCs can occur.
Portal Hypertension Diagnosis
- Diagnosis is made by the presence of : Splenomegaly, Ascites, Encephalopathy, Oesophageal varices.
- Varices are seen by fiberoptic oesophagoscopy.
- MRI (Magnetic resonance imaging) and CT (Computerized tomography) also show collateral circulation in portal hypertension.
- Portal venous pressure can be measured directly by skinny needle catheterization i.e. direct insertion of’ needle through skin to the hepatic veins.
- The wedged hepatic vein pressure is increased in sinusoidal and post sinusoidal portal hypertension (cirrhosis).
- It is normal in pre-sinusoidal portal hypertension. Mesenteric and hepatic angiography may sometimes be required before portal systemic shunt surgery.
Portal Hypertension Treatment
- Surgical decompression may be done to lower portal pressure.
- Decompression without surgery may be done by TIP-transjugular intrahepatic portosystemic shunt.
- Beta blockers such as propranolol, nadolol cause vasoconstriction and reduced cardiac output and reduce bleeding.
- HVPG (Hepatic Venous Pressure Gradient) = Wedged Hepatic Venous Pressure Minus Free Hepatic Venous Pressure.
- HVPG must be reduced to less than 12 mmHg
- Portal hypertension due to cirrhosis is not reversible. In alcoholic hepatitis and cirrhosis, chronic active hepatitis and other liver diseases, intensive treatment can give good results.
